In this article, I discuss everything you need to know about celiac disease, from how it’s diagnosed to how it’s treated and managed. I’ve lived with celiac disease for 10+ years and can share my knowledge as both an expert in nutrition and as a patient of celiac disease. This article should not be construed as medical advice and contains affiliate links. Please read my disclosures and disclaimers.
Since you stumbled upon this article, chances are you or someone you know has celiac disease.
I was diagnosed with celiac disease more than 10 years ago and have learned a lot about the disorder in that time.
I think my experience and expertise as a patient of celiac disease make me uniquely equipped to help you understand and manage this serious disorder.
What is Celiac Disease?
Celiac disease is a genetic autoimmune disease that affects about 1 in 100 people, which is about one percent of the population.
When someone has celiac disease, their immune system becomes confused and mistakenly attacks the healthy tissue surrounding the small intestine whenever they eat gluten, a protein found in wheat, rye, barley, and sometimes oats.
The attack is swift and constant. Over time, the person’s microvilli, or the hair-like follicles surrounding the small intestine, become damaged and flattened. This is known as villous atrophy.
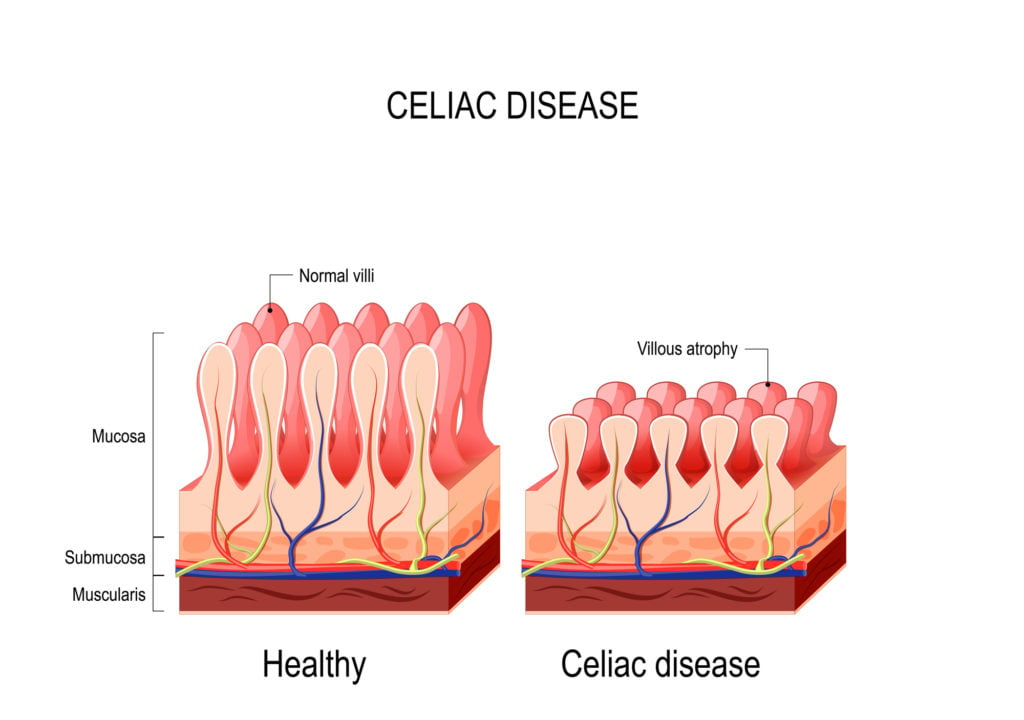
What most people don’t realize is that the small intestine is a vital organ that feeds every other organ and cell in the body. In other words, without a properly functioning small intestine, a person can become malnourished and nutrient deprived, all of which can lead to various disorders throughout the body.
There are dozens of symptoms related to celiac disease beyond the classical gastrointestinal symptoms (bloating, gas, diarrhea, etc.) that most people associate with the disease. These symptoms include but are not limited to the following:
- Nutrient deficiencies (anemia, Vitamin B deficiency, feeling shaky between meals)
- Osteopenia or osteoporosis
- Fatigue
- Joint pain or arthritis
- Weight loss
- Diarrhea
- Constipation
- Bloating
- Chronic gas
- Failure to thrive and short stature (children)
- Dental (enamel) issues
- Irregular menstruation
- Fertility issues
- Depression, anxiety, or other mental and/or behavioral disorders
- Dermatitis herpetiformis (also known as celiac rash)
- Hair loss
- Oral issues (canker sores, geographic tongue)
Some people experience what is known as silent celiac disease, which means they have no blatant celiac symptoms, yet they have an autoimmune disorder.
Testing and Diagnosing Celiac Disease
Celiac disease can be diagnosed (by a doctor) using a simple blood test. Many people will take an at-home celiac disease screening test (pictured below), then discuss the results with their doctor.
If the test is positive, they likely have celiac disease, and many physicians will follow up the blood test with an endoscopy procedure to biopsy and examine the small intestine.
If a blood test is negative, but a person suspects they have an issue with gluten, a doctor might recommend that they go on an elimination diet to see if they’re gluten intolerant instead. Read Do You Have Gluten Intolerance? How to Test for Non-Celiac Gluten Sensitivity for more information on testing for non-celiac gluten disorders.
My blood test was positive for celiac disease. I then visited a GI doctor who biopsied my small intestine and confirmed celiac disease. This is the gold standard method for testing for and diagnosing celiac disease.
Is Celiac Disease Genetic?
Celiac disease is a genetic disorder, and people with celiac disease carry either or both the HLA-DQ2 or HLA-DQ8 genes.
Research shows that people with a first-degree relative with celiac have a higher risk of getting the disease, and siblings of first-degree relatives have the greatest genetic risk.
You can undergo genetic testing to determine if you carry one of the celiac disease genes. You can also take this at-home genetic test (pictured below) to see if you carry one of the two celiac genes.
Celiac disease can turn on at any time in genetically predisposed people. This means someone with one of the celiac genes might test negative for celiac disease one day and, years later, test positive. Genetic screening can help determine whether annual celiac disease screening is necessary.
I tested both of my kids for the celiac gene. My son doesn’t carry either gene, but my daughter carries one of the genes (the same one I carry). This means I will need to screen my daughter for celiac annually, but not my son.
Just because someone has one of the celiac genes does not mean they have or will get celiac disease, although Dr. Tom O’Bryan says in his book, The Autoimmune Fix, that gluten intolerance is a precursor to celiac disease in genetically predisposed people.
What Causes Celiac Disease?
While you must have a genetic predisposition to celiac disease to have the disorder, researchers have found that two additional factors must also be present.
First, you must also be eating gluten (obviously), and second, you must experience some intestinal permeability (leaky gut), which is often triggered by poor eating habits, viruses, trauma, antibiotics, or a weakened immune system.
When someone with celiac stops eating gluten, their symptoms resolve with some exceptions, like those with non-responsive refractory celiac disease.
In many people, celiac disease develops over time, with gluten slowly damaging the small intestine like a leaky faucet. Eventually, after years of eating gluten, the pipe bursts, and poof, a person has full-blown celiac disease.
Testing for Celiac Disease
Getting tested for celiac disease requires a simple blood test that can be performed by a doctor or discreetly at home using this celiac disease screening test.
If the test is positive, a doctor may want to perform an endoscopy procedure to biopsy the small intestine and look for damage consistent with celiac (flattened villi and inflamed small intestine lining).
If the blood test is negative, the doctor might want to evaluate a person for non-celiac gluten sensitivity, perform a celiac disease genetic test, or look for other related disorders like acid reflux, IBS, Crohn’s, SIBO, candida, etc.
I suggest reading Do You Have Gluten Intolerance? How to Test for Non-Celiac Gluten Sensitivity. Most experts say if you suspect you have an issue with gluten, you should do an elimination diet for 4-6 weeks. Alternatively, Dr. Tom O’Bryan, author of The Autoimmune Fix and leading gluten-sensitivity doctor, recommends the Cyrex Array 3x or Wheat Zoomer tests.
Managing Celiac Disease
I can attest that managing celiac disease is a bear and something a person can never take a break from doing. Currently, the only treatment option for celiac disease is a strict gluten-free diet.
Despite not being able to eat gluten, people with celiac disease can still enjoy a variety of naturally gluten-free foods, including fresh fruits and vegetables, cheeses, meats, fish, eggs, beans, potatoes, lentils, and various gluten-free grains, including rice, buckwheat, and quinoa, as well as these 200+ Foods You Can Eat on the Gluten-Free Diet.
While a whole foods diet is best for those with celiac disease, it’s not always easy to do, and many people want to enjoy packaged foods or eat at restaurants from time to time.
Unfortunately, gluten is found in many confusing ingredient labels and hidden foods, like soy sauce and licorice. This is why label reading is one of the most important skills a person with celiac disease can master.
Many restaurants don’t understand the ins and outs of creating a safe, gluten-free meal free and that even a crumb of gluten can hurt their gluten-free customers. This is why learning to eat out safely is top of mind for many people with celiac disease. I recommend downloading The Ultimate Guide to Eating Out Gluten Free for information on how to eat out as safely as possible.
Long-Term Prognosis for Celiac Patients
For those following a gluten-free diet and properly managing their symptoms, the prognosis is good.
Many people (including me) have put their celiac disease symptoms into remission by adhering to a strict gluten-free diet. While the disease will never go away, it can become dormant.
However, many individuals struggle to fully adhere to a gluten-free diet, especially since gluten is addictive.
Dr. William Davis, in his New York Times best-selling book, Wheat Belly, talks about gluten’s opiate-like effect on the brain. He says wheat is hard to give up and causes distinct withdrawal symptoms in those who stop eating it. While the gluten-free diet is the only treatment option for people with celiac disease, it also is a difficult treatment regimen for many to follow.
On top of that, some people suffer from gluten cross-contamination or occasionally get accidentally glutened. Some don’t take their disorder seriously and choose to cheat on their gluten-free diet.
Unmanaged (or improperly managed) celiac disease can lead to additional autoimmune diseases, fertility issues, worsening and painful symptoms, and serious, life-threatening diseases such as cancer, particularly intestinal lymphoma and small bowel cancer. Commonsense says anyone living in a chronic state of inflammation is ripe for disease.
A study published in Gastroenterology said that the later in life someone is diagnosed with celiac, the higher their risk of getting additional autoimmune diseases. This is one of many reasons early detection of celiac disease is crucial.
Living with Celiac Disease
Celiac disease is a lifelong affliction that must be continually managed via a strict, gluten-free diet. Currently, there is no cure for celiac.
As someone who lives with celiac daily, I uniquely understand the challenges. The daily struggle and emotional burden of the gluten-free diet are real. It’s not easy to eat out, travel, shop for groceries, or eat at a friend’s house. You must always find ways to balance dietary vigilance with the day-to-day realities of life.
Eating with friends and family is the fabric of Western culture. Most social plans revolve around food. I’ve spent many years figuring out ways to mitigate the risks of eating out and getting sick from accidental gluten exposure. I share my full story in my book, Dear Gluten, It’s Not Me, It’s You. I also wrote an ebook called The Ultimate Guide Out Gluten Free, showing you how to eat out safely.
I also occasionally use a Nima Sensor, the portable gluten-detecting device pictured below, to help me eat out safely and decode packaged foods for hidden gluten. Please read my article, What You Need to Know About Nima Sensor Before You Buy.

I believe you can live a healthy, happy life with celiac, but you must always be vigilant and aware of everything you eat. Labeling reading, advocating for yourself, and communicating the seriousness of your diet can help you mitigate the risks of accidentally eating gluten.
Celiac disease has a high treatment burden that requires a person to overhaul and restrict their diet. And while many people with celiac disease agree that it’s nice not to have to depend on pharmaceutical companies to help manage their disease, the burden of the gluten-free diet weighs heavily on the community.
Need Help Going Gluten-Free?
- Enroll in my SIGNATURE Gluten-Free Course
- Read my 10 Tips to Getting Started on a Gluten-Free Diet
- Take the Gluten-Free Made Easy Course I created with Dr. Tom O’Bryan
- Purchase my book, Dear Gluten, It’s Not Me, It’s You
- Visit my Celiac Disease Library
Leave a Comment