
In this article, I highlight gluten and its connection to underlying mouth disorders such as canker sores, cold sores, geographic tongue, and tooth enamel defects. No information in this article should be used as a substitute for medical advice from a doctor. This post contains affiliate links. Please see my disclosures and disclaimers.
Before I was diagnosed with celiac disease 10+ years ago, I suffered from a slew of embarrassing mouth issues. I had canker sores, occasional cold sores, and roaring geographic tongue.
These conditions were sometimes painful and always embarrassing, and I didn’t know what caused them to occur in the first place. I was only a kid when I first experienced these mouth ailments, which continued well into my adult years.
I’ve learned that mouth sores are often oral manifestations of more serious, underlying disorders. My mouth disorders told me something wasn’t right in my body, particularly my gut. And with time, I learned that the condition at play inside of me was celiac disease.
Celiac disease is a genetic autoimmune disorder that affects 1 in 100 people worldwide. When a person with celiac disease eats gluten, a protein found in wheat, rye, barley, and sometimes oats, their immune system becomes confused and mistakenly attacks the lining of the small intestine.
The disorder is devastating because the small intestine is crucial for nutrient absorption and distribution; it feeds all the other organs and cells in the body. Without a properly functioning small intestine, a person can become malnourished and vitamin-deficient, which puts them at high risk of a slew of symptoms, diseases, and even early death.
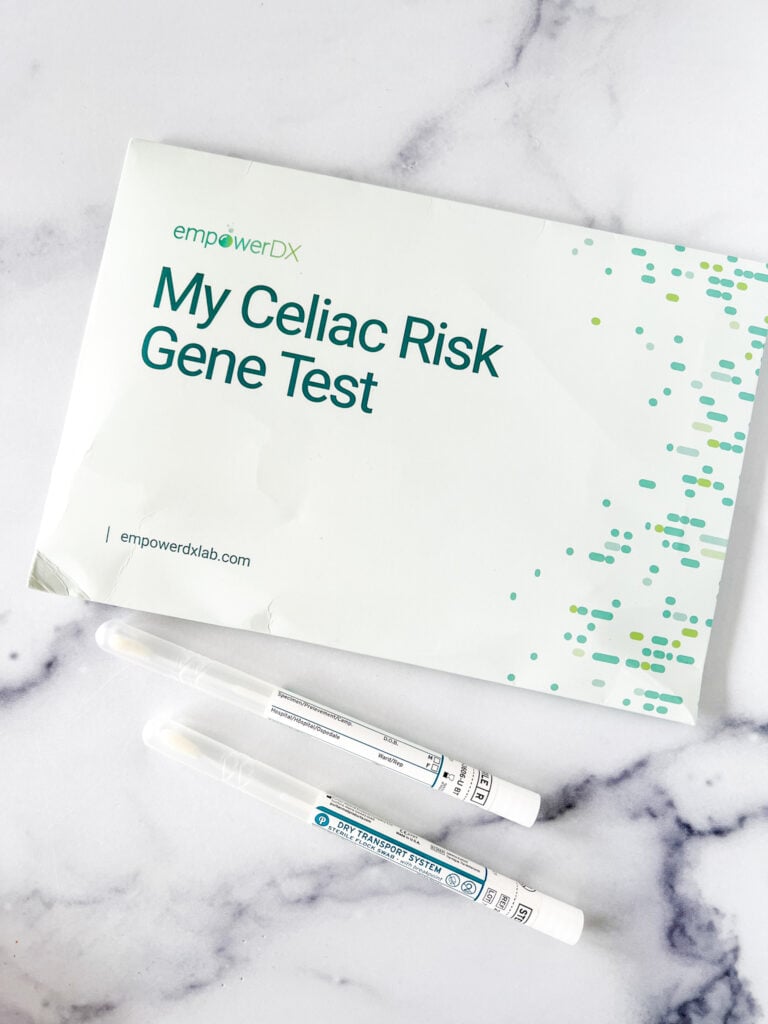
In this article, I discuss various mouth disorders and dental manifestations of a gluten disorder or celiac disease. If you experience any of these mouth disorders and suspect you might have an issue with gluten, either talk to your doctor about getting tested for celiac disease or take this at-home celiac disease test and discuss the results with your doctor.
Canker Sores and the Gluten Connection
Canker sores are known as recurrent aphthous stomatitis (RAS), and they’re found on the soft tissues inside the mouth, lips, cheeks, and tongue. Canker sores can be painful, but they aren’t viral nor contagious like cold sores.
While the exact trigger of a canker sore is unknown, many experts say a vitamin deficiency (iron, B12, and folate), weak immune system (hello celiac disease!), food sensitivities, and hormonal changes all potentially contribute to the disorder.

In a 2020 study, researchers found children with celiac disease to be three times more likely to experience recurrent mouth ulcers. Another study found a significantly higher prevalence of canker sores in patients with celiac disease than in the general population.
Even patients with non-celiac gluten sensitivity (NCGS) experience a higher prevalence of canker sores. In a study of patients with NCGS, researchers fed participants low doses of gluten to assess their symptoms. They found gluten intake significantly increased the prevalence of aphthous stomatitis (canker sores) compared with those taking the placebo.
Based on these data, both people with celiac disease and NCGS are more likely to be afflicted with canker sores, highlighting the need for vigilance to the gluten-free diet and a call for people with canker sores to get tested for celiac disease and non-celiac gluten sensitivity.
Cold Sores and the Gluten Connection
Cold sores are inflamed blisters caused by a virus called herpes simplex virus. They typically occur on the external surfaces of the lips, although they can also occur on the nose, cheeks, or eyes. They often occur in the same spot and emerge when the nerve is triggered, typically by stress or illness. They might also be a sign of an underlying immune disorder.
Cold sores last 2-4 weeks and are contagious when active. It’s wise to avoid touching lips, kissing, or sharing drinks during an outbreak to prevent spreading the virus to others.
Cold sores are more common than most people realize; ninety percent of all people have had at least one cold sore in their lifetime. Fortunately, many people develop antibodies to cold sores after their first one and never have to deal with them again. About 40 percent of the population experience recurring cold sores. Why the virus afflicts some more than others is unknown.

Unfortunately, no studies correlate gluten consumption to cold sores; however, researchers have found clues that implicate viruses as triggers of celiac disease. Researchers have identified a connection between celiac disease and viral disorders such as Epstein-Barr Syndrome (mono), reovirus, rotavirus, and adenovirus.
Anecdotally, I get cold sores more infrequently now than I did in my pre-celiac years, perhaps because I have strengthened my immune system, healed my gut, addressed underlying nutritional deficiencies, and put my celiac disease symptoms into remission.
Geographic Tongue and the Gluten Connection
Geographic tongue, or benign migratory glossitis, is an unexplained phenomenon inside the mouth. The condition gets its name from the map-like appearance on the tongue’s top and side. The condition looks like crop circles on the tongue.
The cause of geographic tongue is unknown, although some consider geographic tongue an oral form of psoriasis. Geographic tongue affects 1-3 percent of the population, and unlike cold sores, it’s not viral nor contagious. I can attest that geographic tongue feels like your tongue is chronically inflamed.

Since childhood, I’ve asked every doctor and dentist about my geographic tongue. Each doctor and dentist told me not to worry about it because “it’s nothing.” In other words, it was just something I had to live with, and they knew little about why I had it or what caused it.
The truth is, my geographic tongue was likely an early sign of celiac disease, and evidence suggests there is a strong tie between the two disorders.
One study found that 15 percent of individuals with geographic tongue had celiac disease, which is 15 times the rate of celiac disease in the general population!
On top of that, only a fraction of the 15 percent of patients with geographic tongue had any gastrointestinal symptoms. This means that individuals with geographic tongue may experience “silent” or “atypical” forms of celiac disease.
Research suggests that any inflammation in the mouth, geographic tongue included, may be caused by a vitamin B12 deficiency, which is a known vitamin deficiency in people with unmanaged or undiagnosed celiac disease.
Please read Geographic Tongue (Glossitis) and the Gluten Connection for more details on how these two disorders are connected.
Tooth Enamel Damage and Celiac Disease
In a 2023 study published in Nature, researchers found a link between tooth enamel damage in people with celiac disease and the appearance of autoantibodies.
Most experts previously believed that dental manifestations in celiac disease were caused by malabsorption issues due to gut inflammation; however, this research shows that tooth enamel defects and damage may be caused by specific antibodies found in people with celiac disease.
These specific antibodies interfere with enamel formation, and it’s why tooth enamel fails to properly develop in some children with celiac disease.
Preventing Mouth Sore Outbreaks
If you suffer from any of these mouth sores, consider the following:
(1) Get Tested for Celiac Disease: If you experience any oral disorders discussed in this article, get tested for celiac disease before going gluten-free. You must be eating in order for a celiac disease test to be accurate.
Don’t want to visit the doctor? I highly recommend this at-home celiac disease screening test as an excellent first step.

(2) Go Gluten-Free: If you don’t have celiac disease but suspect you have non-celiac gluten sensitivity or gluten intolerance, go on an elimination diet. Eliminate gluten from your diet for 4-6 weeks, then slowly reintroduce it and see how you feel and if your mouth and dental issues reemerge.
Be strict about your elimination diet – no cheating! Even small or accidental gluten exposure can sabotage your intestinal health and put the experimental elimination diet in peril.
(3) Evaluate Nutrient Levels: Since mouth sores may also be a sign of Vitamin B or D or other nutrient deficiencies, be sure to follow a diet rich in anti-inflammatory foods. Consider taking a daily supplement – read Supplements for Celiac Disease and Gluten Intolerance to learn more about which ones I recommend.
You can also evaluate your nutrient levels with an at-home nutrient-check test. There are at-home tests that can check your Vitamin D and Vitamin B levels.
(4) Mind Your Gut Health: Remember, the mouth is the gateway to your gut. Improve your gut health, and you’ll improve your whole body – and mouth – health. Read about the benefits of probiotics and the connection between gluten and a leaky gut.
(5) Don’t Ignore Oral Symptoms: Celiac disease can manifest itself in many ways. Even if you don’t have classic gastrointestinal symptoms traditionally associated with celiac disease, it doesn’t mean you don’t have the disorder.
If you suffer from mouth disorders but don’t have celiac disease, consider undergoing genetic screening for celiac disease. This at-home cheek swap test will reveal if you carry the celiac gene(s). If you do, you’ll want to get screened for celiac disease annually.
(6) Take Care of Yourself: Stress and illness can trigger canker sores, cold sores, and geographic tongue. Eat well, sleep well, be physical, and reduce stressful activities. These behaviors will serve your body well and keep you feeling your best.
Please Share Your Experiences
Do you suffer from any of these oral disorders? Did your symptoms improve upon implementing a gluten-free diet? Please share your stories in the comments below to help others.
Additional Reading
Enjoy these related articles:
- Geographic Tongue (Glossitis) and the Gluten Connection
- What to Expect When Getting Tested for Celiac Disease (Blood Test and Endoscopy)
- Is Gluten Intolerance a Precursor to Celiac Disease?
- Do You Have Gluten Intolerance? How to Test for Non-Celiac Gluten Sensitivity
- Can Celiac Disease Cause Hair Loss?
I have always had issues with canker sores, I have leaky gut and cannot eat gluten, corn or soy. I still have peeling inside my mouth, but I also have almost nonexistent folate levels while taking folate supplements for 2 years now and B-12 shots in my stomach to maintain B-12 levels.
I had problems with canker sores in my mouth for years, but by process of elimination figured out it was the sodium laurel sulfate in just about every toothpaste I checked. I finally started using a toothpaste for sensitive teeth, with no SLS. It greatly reduced the frequency of the canker sores. I now make my own tooth powder, to be able to choose each of the ingredients.
Now, with celiac disease, and on a 100% gluten free diet for the last six years, I very seldom have one pop up. They do seem to be triggered if I inadvertently bite my lip or inside cheek, though.
Thanks for the useful information!
Jenny, you are a wealth of knowledge. Your book is wonderful too.
I never realized that the sores I’ve been getting all my life, and I’m 70!, would have anything to do with my celiac disease. Although we try very hard here, my family still deserves their bread and desserts. I just never thought, even though I did not eat, the contamination would get me. Thank you for bringing this subject to us. I truly appreciate it and you!.
Jenny, thank you for letting your readers know about the gluten and canker sore connection. I had such awful painful sores all my life until I went gluten free. After many gf years of being canker free, I recently started getting cankers on my tongue. I discovered a connection between the sores on my tongue with nsaid use. Every time I need to use an nsaid (such as Motrin) for more than one dose, I will get a canker sore on my tongue. I never had them on my tongue before. Just something for people to look out for as another possible cause.
It could be the sign of a nutritional deficiency and it will take time for your body to recover. It took years for my tongue to fully clear and my body to heal.
interestingly, I was just diagnosed with celiac a few weeks ago and have had so many issues with my tongue. I have always had an “ugly” tongue but it never caused the sores or pain until about a month ago. I was eating gluten like crazy to ramp up for my scope. I have been gluten free for about 2 weeks and its not going away exactly. What makes it go away? I am on a plethora of pro/prebiotics and vitamins to heal my gut, they probably arent being absorbed until there is more healing I supposed. I have on occasion gotten Canker sores, but it was not often, maybe 1 a year or less and usually wasn’t a big deal and would go away in a day or two. I don’t recall every having a cold sore, but my sister gets them.
This is an interesting article. I’ve had cold sores for as long as I can remember. I was getting them at least every few months. I had 2 bad cold sores when I was first diagnosed. I was so stressed from the diagnosis. Then it was over a year afterwards before I had another one. That was unheard of for me. I just had one (15 months after going GF). It was very mild compared to my normal ones. Another positive benefit to add to the list for not having gluten.
Wow, I’m glad I could help you connect the dots. Our bodies are intricately intertwined. What happens in the mouth can be caused by something happening in you gut. Be well friend!
Thank you for this article. I was diagnosed this past August 2019. I have lived with a bad stomach, constant cold sores, canker sores my whole life. This past spring my dentist hygienist mentioned I have geographical tongue. I had never heard of it before her mentioning it and then I read this article. Everything makes sense now. I am B12 deficient and many other deficiencies. Since being diagnosed I hadn’t had a cold sore until a week ago and I do believe I was crossed contaminated from the restaurant I ate at or the bakery that I bought a gluten free cake from. They claimed they watched how they made it as far as cross contamination, but I definitely was sick that night and the next day I had sores in my mouth, sores on my neck and a cold sore. I look forward to reading more of you articles. Thank you again.
I’ve had huge cold sores on my mouth and nose, at least one a month between October and March every year from early twenties until winter before last when I was 68. Nothing I tried helped. I went gluten free about 10 years ago and have never been tested for celiac disease but am definitely gluten sensitive. I stopped eating gluten after reading the Wheat Belly book by Dr. Davis. As soon as I went GF have been pretty careful to not eat gluten, but possibly will try to be even more careful. I also had trouble with large “pimples” that were painful on my face which have gone away.
I also get a small blisters on my tongue and they are very painful. I only get them when I have eaten gluten. I m gluten sensitive and have noticied it when I have eaten gluten more than a cheat.
Thank you for sharing Deb. Im glad you figured things out. I hate hearing of people suffering and hopefully together we can bring more attention to this important topic.
I read your articles and always find something I didn’t know . I had cold sores since childhood. I don’t mean one or two, I mean sometimes my mouth would be covered inside and very painful. Naturally my Mom thought I was very skinny because I couldn’t eat. The dentist had no idea except I should avoid citrus, acid such as tomatoes etc. Didn’t help. It wasn’t until adulthood that my gut hurt so bad I couldn’t eat my chicken noodle soup. I had diarrhea so bad , I dreaded going out. My abdomen was so bloated and hard, I had to lie down many times during the day. My arthritis started in my twenties and got so bad in my fifties. To make a long story short, I only get mouth sores when glutened . I never cheat. I mean never. Nothing not even homemade chocolate cake. So chalk the nugget of mouth sores up as more info is knowledge. Thank you