
A strict gluten-free diet is the only treatment protocol for people with celiac disease and non-celiac gluten sensitivity. While vigilance to a gluten-free diet has been proven to improve a person’s health outcomes, hypervigilance has been shown to impair one’s quality of life. In this article, I share what researchers found when they examined this topic and how a person can balance dietary vigilance with quality of life. Please see my disclosures.
People with celiac disease and non-celiac gluten sensitivity must follow a strict, lifelong gluten-free diet free from gluten, a protein found in wheat, barley, rye, and sometimes oats.
Even a crumb of gluten can create symptoms and damage in a person with celiac disease, an autoimmune disorder affecting 1 in 100 people worldwide. Gluten also can lead to widespread inflammation in people with non-celiac gluten sensitivity.
The gluten-free diet is the only treatment option proven to help celiac patients achieve symptom, serological, and histological improvement and deter future diseases caused by villous atrophy.
Villous atrophy occurs when the villi surrounding the small intestine become flattened or eroded. The villi are essential for nutrient absorption, and it’s why many people with undiagnosed celiac disease suffer from nutrition-related disorders and complications.
While several studies, including this one and this one, suggest that good adherence to a gluten-free diet will lead to symptom resolution and significantly improve one’s quality of life, it’s no secret that the treatment burden is high for the celiac community when compared to other disorders.
The gluten-free community must constantly scrutinize food labels to identify hidden gluten in food, medications, supplements, makeup, toothpaste, lip balm, sunscreen, etc.
The community must also be vigilant about sources of airborne flour, using shared appliances such as convection ovens, air fryers, and toasters, and exercise extreme caution when eating out, given that one in three gluten-free labeled restaurant dishes contains detectable levels of gluten.
On top of it all, the gluten-free community must navigate complex food environments such as cruises, traveling, colleges, summer camps, and professional events, and gracefully navigate a steady stream of social situations where food is inevitably part of the plan.
Examining Gluten-Free Hypervigilance
In 2017, researchers looked into the potential negative consequences of a strict gluten-free diet in a study titled “Hypervigilance to a Gluten‑Free Diet and Decreased Quality of Life in Teenagers and Adults with Celiac Disease.”
Researchers examined how different adherence levels and knowledge about the gluten-free diet affected one’s quality of life. The study involved 80 adult and teenage participants, all with a biopsy-confirmed celiac disease living in a major metropolitan area.
The researchers assessed how well the participants were adhering to the gluten-free diet and classified them into one of two categories:
(1) Those with “excellent adherence” to the gluten-free diet were categorized as “extremely vigilant.” These are participants who ate at celiac-friendly restaurants, asked thorough questions when dining out, and eliminated cross-contamination in their kitchens. [Is it just me, or is it unfortunate that the researchers used the words “extremely vigilant” to describe participants with “excellent adherence” to the gluten-free diet?]
(2) Researchers tagged a second group of participants as “less vigilant.” These participants were more relaxed in their approach to a gluten-free diet.
Researchers concluded that “extremely vigilant” participants experienced a “significantly lower” quality of life than their less vigilant counterparts, noting that “quality of life” is a subjective term.
In prior studies, researchers classified healing and symptom resolution as a quality-of-life measure. However, these researchers defined quality of life based on dietary adherence without consideration of health outcomes.
While the research is flawed, it does highlight a conundrum faced by the gluten-free community: How does a person with celiac disease balance the necessity and reality of a strict gluten-free diet without significantly lowering the quality of their life?
I’ve given great thought to this conundrum over the years and have concluded that many people are too gluten-free, and they follow a diet beyond what is necessary to live a full, healthy, and sane life without gluten.
Balancing Vigilance with Quality of Life
Below, I share ten tips for achieving good dietary adherence without losing your mind or lowering the quality of your life.
My tips are subjective, and some people must be stricter than others to feel well.
However, most of the celiac community can heed these tips to balance the psychological and physical burdens of a gluten-free diet without sacrificing the quality of their life.
(1) Reduce Your Reliance on Eating Out, But Don’t Stop Eating Out
I used to eat out all the time, and my busy life didn’t lend itself to cooking at home. Then, enter celiac disease. It turned my life upside down and reminded me that the status quo wasn’t working.
When you’re diagnosed with a gluten disorder, your body is telling you that you need to slow down, and one of the ways you can do this is by taking time to prepare meals at home, which will always be the safest and healthiest option. (Meal planning is your friend!)
However, you can and should still eat out. Anyone who admonishes you for eating at a restaurant doesn’t live in the real world.
If your coworkers are going to lunch to celebrate the boss’s birthday, you should go.
If you want to attend a conference or visit Spain, you should do these things and not let your “disability” control your life.
The key is to reduce your reliance on eating out and do so only when the occasion calls for it.
Spend time learning how to prepare simple, fast, and health-forward meals at home so you can fuel and nourish your healing body and lessen your risk of getting accidentally glutened by well-meaning restaurants that still get gluten-free wrong.
(2) Use a Portable Gluten-Detecting Device
The researchers in the Hypervigilance study suggested using a portable gluten sensor to help you feel more comfortable eating out.
I agree that such tools can be extremely helpful in giving you confidence that, yes, the burger that looks too good to be true is safe to eat.
However, any gluten-detection tool, whether it be Nima Sensor or a gluten-detecting dog, comes with limitations in what it can and can’t detect (read about Nima’s limitations). And it’s open to translation whether these tools foster food freedom or food fear. (The answer can be both!)
For example, should Nima or a gluten-detecting dog find gluten in a dish, a person would need to have an uncomfortable and awkward conversation with their waiter.
For some, this is par for the course; for others, it’s an anxiety-inducing nightmare.
For some, Nima gets them out of food jail and helps them eat more freely and confidently; for others, it creates unnecessary stress and anxiety at the table. The community must weigh the pros and cons of such tools.

(3) Surround Yourself with Supportive People
Having supportive family and friends makes the gluten-free lifestyle less isolating and burdensome. I often need my friends and family to help me manage the never-ending burdens of a gluten-free diet.
After a long day of skiing, my family and I went to Chipotle. There was a long line; I knew I would hold up the line when I asked the staff to wash hands, change gloves, and get fresh ingredients. (See my Chipotle post for tips on ordering gluten-free at Chipotle). I didn’t want to order anything.
My young daughter wouldn’t let me off the hook so quickly. She told me I deserved to eat my usual burrito bowl, and it would only take an extra minute for the staff to comply with my request.
She was going to order for me to make sure I ate. I needed this extra nudge from someone who loves and supports me.
I have a friend who takes it upon herself to explain to the waitstaff the seriousness of my diet, relieving me of this heavy burden from time to time.
Another friend stared down a short-order cook as he prepared my burger, telling him what to do and ensuring he got it right. She even gave him a tip, without my knowledge, to ensure he took care of me.
(4) Don’t Obsess Over Good vs. Bad Foods
People with celiac disease are also at risk of orthorexia, a hyper-focus on eating in a specific, proper, or healthful way.
While orthorexia isn’t classified as an eating disorder (yet), many experts consider it a form of disordered eating, especially when a gluten-free diet becomes hyper-restrictive and begins to negatively impact the person’s quality of life.
Be careful not to label foods (outside of gluten) as “bad.” Don’t get caught up in paleo, keto, low-carb, and grain-free diets. Steer clear of cleanses, detoxes, and other diet-culture nonsense.
Instead, eat in a way that feels good without depriving yourself of your favorite foods. If you want a [gluten-free] cupcake, eat one.
I strive to eat whole and nourishing foods 85 percent of the time, and when I crave potato chips and want to sneak a handful of chocolate chips, I do it. Strive for balance, not perfection.

(5) Trust Labels (Unless Given a Legit Reason Not To)
Over the years, I’ve met thousands of gluten-free people, and many say they won’t eat anything not labeled gluten-free. Others say they won’t touch food unless it’s labeled “certified gluten-free,” where a third party, like the GFCO, verifies the product contains less than 20 parts per million (ppm) of gluten per the FDA’s gluten-free labeling ruling.
When a product is labeled “gluten-free,” it’s safe to eat, and avoiding it is an unnecessary restriction. When a company labels a product “gluten-free,” it contains less than 20 ppm of gluten.
Even if a product contains 19 ppm of gluten, a person with celiac would still be okay eating it.
In fact, researchers say a person could consume 300 grams of gluten-free products, each containing 20 ppm of gluten, and remain safely below the 10 mg threshold of daily gluten.
Ten milligrams is the widely accepted amount of gluten a person with celiac disease can safely eat daily without causing intestinal damage. (Read: Is the FDA’s 20 ppm Gluten Threshold Enough? for more details on this complex topic.)
Unfortunately, even food manufacturers are fallible, and some products contain more gluten than is legally allowed.
The Gluten-Free Watchdog once found levels above 20 ppm of gluten in certified gluten-free oats from GF Harvest and certified gluten-free granola from Safe & Fair.
I have found detectable levels of gluten (using the Nima Sensor) in PB Fit and Progresso soups. (Remember that I have no way of knowing if Nima found gluten above or below the 20 ppm gluten threshold, which is one of the device’s limitations.)
The vast majority of gluten-free and certified gluten-free labeled products, even Cheerios, are just fine to consume when following a strict gluten-free diet.
When an exception comes to light, you should avoid that product. But don’t let it deter you from enjoying other “gluten-free” labeled foods.
If you eat a product that makes you sick, contact the manufacturer to verify that it’s testing its products before labeling them “gluten-free.” Ask to see the company’s testing data to confirm any gluten-free claims.
(6) Don’t Let Some “May Contain” Statements Stop You
Per the Food Allergen Labeling and Consumer Protection Act of 2004 (FALCPA), food manufacturers must provide disclosure, in plain English, if their products contain any of the top eight food allergens, including wheat, soy, milk, eggs, tree nuts, peanuts, shellfish, and fish.
Please note that manufacturers are not required to disclose if their products contain barley and rye, which also contain gluten. FALCPA requires only wheat disclosure.
(Update! The Food Labeling Modernization Act of 2023, if passed, will require food manufacturers to disclose all sources of gluten.)
Because food manufacturers are required to disclose the presence of wheat in foods, you’ll see statements at the bottom of food labels that say:
- May contain wheat.
- Produced on equipment used to produce products that contain wheat.
- Produced in a facility that also produces products that contain wheat.
Avoid: Products that may contain wheat and products that are produced on shared equipment (without a gluten-free label).
The box of Cocoa Puffs pictured below doesn’t list any gluten ingredients in plain English in the ingredients, but its “May Contain Wheat Ingredients” disclosure should have you putting this product back on the shelf.
Keep in mind, however, that many certified gluten-free products are produced using shared equipment and manufacturing facilities. These products are safe to consume on a gluten-free diet.
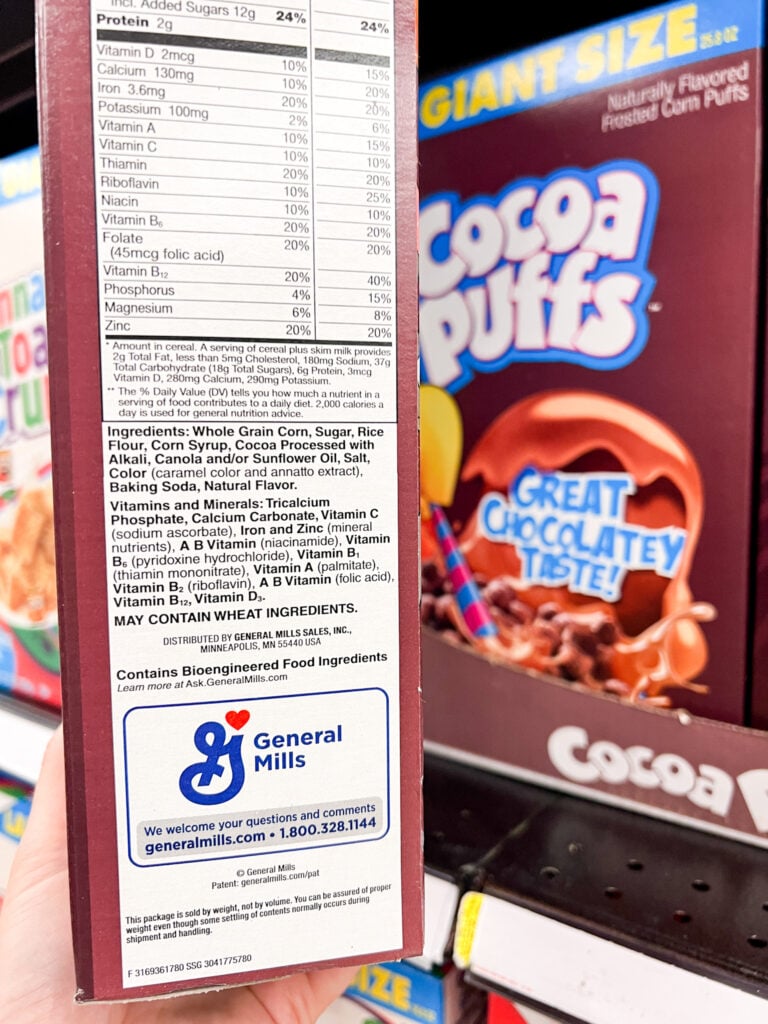
Consider: Avoiding foods made in a shared facility would be another unnecessary restriction. Manufacturing facilities are enormous, and a product made in the same facility as a product that contains wheat is unlikely to come in contact with wheat.
Such products are generally considered safe for the gluten-free community (of course, look for other clues on the label).
(7) Eat [Gluten-Free] Oats
Nothing stirs up controversy in the gluten-free community than whether or not you should eat oats.
Oats are naturally gluten-free; however, they are produced in shared wheat fields using shared equipment and are cross-contaminated with wheat.
For more information on oats, read Are Oats Gluten Free? Unpacking Confusing and Contradictory Information.
Major companies have found a way to optically or mechanically sort and cleanse the oats of all gluten debris and dust. These oats are labeled “gluten-free” and are generally safe for the gluten-free community.
Of course, there are rare cases where someone has an oat allergy or experiences a phenomenon known as cross-reactivity. These individuals should avoid oats.
However, most people with celiac disease or non-celiac gluten sensitivity can and should enjoy oats. They’re loaded with soluble fiber, which helps to move food through the digestive system, bulk up and soften stool, and deter constipation.
Oats taste good and add texture and structure to many beloved gluten-free products, including gluten-free Oreo cookies, Cheerios, and Girl Scout cookies.
While some experts recommend avoiding all gluten-free oats, everyone must weigh the pros and cons of eliminating yet another food from their already restricted life. Avoiding [gluten-free] oats would once again be an unnecessary restriction.

(8) Take Food Sensitivity Tests with a Grain of Salt
Food sensitivity tests have taken the world by storm, and one of the most popular tests from EverlyWell says it can help you test your IgG reactivity to 204 foods.
After taking the test, people often find out they are “highly reactive” to a dozen(s) of foods. They then implement a never-ending elimination diet that can lead to unnecessary avoidance of a long list of foods, disordered eating, isolation, and emotional angst.
If a food sensitivity test comes back with dozens of foods to avoid, it’s time to consult a doctor, dietician, or another health professional.
Chances are the test is telling you to improve your gut health, and the test is picking up on antibodies your immune system is making to the foods you’re eating (thereby leaking out of your gut and into your bloodstream) and not foods causing actual food intolerances.
Food sensitivity tests often encourage individuals to implement an elimination diet, which can be a helpful practice in determining which foods genuinely bother you.
That said, elimination diets are meant to be temporary, not permanent. A person should eliminate specific food(s) for 4-6 weeks, then slowly reintroduce the foods to assess how each makes them feel.
Too often, individuals permanently and unnecessarily restrict themselves from foods they can eat, leading to a lower quality of life. Read my experiences with food sensitivity testing in this article.
(9) Avoid Negative Discourse Online
I’m often struck by the rampant misinformation in many online gluten-free communities. Some of these ridiculous notions spiral out of control and become rumors and urban legends.
Elissa Goodman is one such spreader of misinformation. I’m sure she’s a lovely lady, and she has celiac disease.
But because she purports herself as a health expert, she must get this right and not tell people with celiac disease that it’s okay to eat gluten as long as you take a digestive enzyme. Nope. Not true.
On top of rampant misinformation, the online community can sometimes be a stew of negativity and judgment, where people on the same proverbial “team” admonish one another for eating gluten-free Oreo cookies because they contain sugar and artificial flavors or call people recommending probiotics “snake oil salesmen,” which they’re not!
Here’s what you need to do to ensure you balance what you need to do to stay safe with the brewing misinformation, disinformation, and negativity brewing online:
(a) Leave Facebook groups and social media sites where negative Nancys are allowed to judge, admonish, and bash people or brands and where this behavior goes unchecked (i.e., the Page facilitator enables these kinds of comments to occur).
Last week, I read comments on a social media post about testing cream cheese. I couldn’t tell if the community was dissing the cream cheese, Nima Sensor, or Nima users that others deemed not intelligent enough to use a Nima Sensor properly.
A more positive way to handle this situation is to teach people how to use the tool correctly to enhance their lives and not allow negativity to flourish. [By the way, Nima says high-fat foods should be tested in small amounts and diluted in water.]
(b) Unfollow influencers who incite anger, anxiety, or exude negative energy. If someone makes you feel bad for doing so, unfollow them. You’ll feel better not seeing their faces in your carefully curated feed.
(c) Not everyone is an expert, even if they have an MD or RD after their name or are part of a legacy organization.
Over the past decade, I think most people can agree that we must challenge the status quo.
No MD writing a study about what I should do has shared my lived experiences. Read 10 Facts Your Doctor Doesn’t Know about Celiac Disease and Gluten Sensitivities for more insights.
(10) Allow Commonsense to Prevail
Above all else, let commonsense prevail. Trust in your knowledge and skills, but be vigilant and careful.
Continually balance the negative consequences of hypervigilance with the negative consequences of getting glutened (aka, sick).
A gluten-free lifestyle requires a tricky balance, but one that can be imperfectly navigated with patience, knowledge, and time.
Did You Enjoy this Article?
If you enjoyed this article, have something to add, or disagree with something I said, please leave a respectful comment below. Your comments help us grow and learn together.
This is incredibly helpful, especially for people learning of a new diagnosis. Social media is a blessing and a curse for learning how to navigate celiac. There are absolutely very vocal folks out there with borderline (or completely) disordered eating habits that steer people away from safe food.
I am in a local FB group that consistently has a few people that refuse to recommend any restaurant for someone with celiac except the small cafe that is dedicated “allergen free” (with erratic hours and limited seating). There are dozens of restaurants in our area that are accommodating, but the message from the group is, unless there is a dedicated kitchen, it cannot be safe for celiac. That is such a limiting perspective.
I like your articles. It’s the hardest thing being gluten free. I rarely eat out and when I do it’s usually breakfast out or a salad with meat. I bring my own dressing. Restaurants don’t care. I was diagnosed about 14 years ago at age 56. I had been so sick for so long and without energy that it was a relief until I started to eat the gluten free way. At the time, very few foods were offered. I got better, but still had the brain fog, thought I was getting alzheimer’s. Then I read the wheat belly book. I had found a recipe for biscuits from the book in a magazine. Anyway, when I read that I gave up all grains too. After a few months, the brain fog and confusion were gone. Along with a lot of inflammation and pain. So I cook almost all my foods. Very happy grain free tortillas are made by la tortilla factory. I’d say I am very vigilant. When I’m not, I’m the only one who suffers. Yes I eat grain free cookies and crackers and chips. Plus sweet potato chips and other things made with no rice flour. Also dark chocolate. Try to avoid mega sugar. But have to have some treats. Just not a lot. Not strictly paleo because I eat potatoes.
Hang in there. This diet is hard and without support, even harder. Sending you a hug from afar.
I stumbled upon your page on Friday during a mental crisis. I’m enjoying your content, I feel seen. I was diagnosed as a 3 yo (positive antibodies, positive biopsy, the whole thing) and I recently turned 23, which means I’ve spent nearly 20 years doing the gluten free diet. I live in Paraguay, in my city of 300.000 people (Ciudad del Este) there isn’t a single restaurant that serves gluten free options, not one. If you get where I’m going with this, 90% of all the food I eat is homemade, but there’s that 10 percent of the time where I really crave the experience of going somewhere, ordering food and eating without having to think about my food. I’m so tired of the constant need to be hypervigilant with food, it’s mentally exhausting and I feel like it puts me on the spot as I don’t really hang out with other coeliacs, so I’m always explaining what the GF life implies (I’ve lost count of how many times I’ve explained cross-contamination)… it’s tiring, and with all of that 2 years ago I discovered a 2nd autoimmunity (my Dr still can’t determine what disease I have, but it manifests as hyperthyroidism with associated antibodies, as well as antibodies associated to hypothyroidism). My point is, I’m so tired at this point that recently I’ve become quite careless with my GF diet, I eat out at cafes that don’t know about cross contamination, I drink the coffee from my university’s Cafe knowing they manipulate food without washing their hands in between touching gluten foods, I eat French fries from McDonald’s… I don’t know where I’m going with this, but I’m struggling and some days I have symptoms so severe I feel like I’m slowly killing myself. I don’t know what to do anymore, I have no support outside of my family
Thank you for your kind words. Oats are an issue for some people on the gluten spectrum due to cross reactivity. The protein in oats mimics gluten and the immune system can become confused. If this happens, don’t eat oats. But the majority of people can safely eat gluten-free labeled oats and should. Restricting oats would be an unnecessary restriction in such cases. Hope that helps. In your case, consider eliminating oats for 4-6 weeks, then reintroducing GF oats and see how you react.
Thank you kindly for your sane, well balanced and educated information. This is the first blog I’ve found that promotes balance and not convincing us to become certified organic dairy free vegan healthy everything no fats no sugar crazy people. I had a question about oats of course. I came across this article about how oats can’t be gluten free and was wondering if you could check it out and tell me your thoughts. I feel like I react to even gluten free oats but I so want to be able to eat gluten free Oreos! Thanks again.
https://www.doctorbecky.net/post/gluten-free-oats-are-not-a-thing
My husband was recently diagnosed Celiac. Moving to a Gluten free existance at such a late age when he didn’t show many serious GI symptoms really had me asking about quality of life. Your common sense information has greatly helped me to relax a bit. Thanks for the helpful tips and resources.
Thank you for your helpful information. I always find help in your emails and articles.
I always enjoy reading your newletter as it is so informative and upbeat.
One of the best articles I’ve read in the 9 months since I was diagnosed with a gluten sensitivity. Thank you.
This article is fabulous. I followed FB groups when I was first diagnosed which resulted in a load of fear on my part. I ended up working for almost a year with a RD that has celiac. It was so worth the money. She taught the same things you have in the article. Nice job!
Thank you Jenny. Your article was right on with what I have experienced in my gluten free journey. I have been gluten free for the past 2 years and it does get easier. Your book is my bible.
Excellent article. I struggle with finding my comfort level eating out. Am getting better with time.
Great article! I really appreciate your logical, thoughtful, and common sense approach to navigating life with celiac. Being newly diagnosed, it’s difficult to balance ‘vigilance’ with simply enjoying life. For others, I can say after a year (since diagnosis) of thinking about food more than I ever wanted to, it does get easier!
You’re so amazing! Thanks for this great article 💜
You are the best! Your articles are always on point. And you are so right about people online.
I am so glad I found someone that I can trust what they say and write!
Thank you!
Thank you so much for your research. I really appreciate how thorough your articles are. I refer back to them often when I need to know what is safe for me as a Celiac.💛