
If you’ve been in the gluten-free community long enough, you’ve likely wondered if the FDA’s 20 ppm gluten threshold is enough and how much gluten a person with celiac disease can consume without getting sick. I discuss these questions and more in this article. This post may contain affiliate links. Please see my disclosures.
Celiac disease is an autoimmune disease in which the immune system becomes confused and mistakenly attacks the healthy tissue surrounding the small intestine every time a person eats gluten. Gluten is a protein found in wheat, rye, barley, and sometimes oats (due to cross-contamination). The only treatment for celiac disease is a strict, life-long gluten-free diet.
While many people in the gluten-free community would benefit from a zero-gluten diet, it’s unrealistic and gratuitous. As you’ll read below, a restrictively low gluten threshold beyond the current FDA’s gluten-free labeling guidelines would add unnecessary complications and potentially limit gluten-free options without improving the overall safety of a gluten-free diet.
In this article, I set out to understand why the Food and Drug Admistionation (FDA) in the U.S. set the gluten-free threshold at 20 parts per million (ppm) and how much gluten a person with celiac disease can safely eat.
I also discuss the limitations of the gluten-free labeling guidelines and why more research is needed to understand how low levels of gluten affect a greater number of people with celiac disease and gluten intolerance.
Understanding Gluten-Free Labeling
Congress passed the Food Allergen Labeling and Consumer Protection Act (FALCPA) in 2004, and the law went into practice in 2006. FALCPA required food manufacturers to disclose on the label, in plain language, if a product contained any of the top eight allergens, which included milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soybeans. These allergens account for 90 percent of food allergies in the U.S.
In 2013, the FDA updated FALCPA to include gluten-free labeling guidelines, which said a product could be labeled “gluten-free,” “without gluten,” “free of gluten,” and “no gluten” when it contains less than 20 ppm of gluten and meets the following criteria:
- It does not contain an ingredient that is a whole, gluten-containing grain (i.e., wheat, barley, rye, or crossbred hybrids of these grains).
- It does not contain an ingredient derived from a gluten-containing grain and has not been processed to remove gluten (i.e., wheat flour).
- It may contain an ingredient derived from a gluten-containing grain that has been processed to remove gluten (i.e., wheat starch) as long as the food product contains less than 20 ppm of gluten.
Keep in mind “gluten-free” labeled foods may actually contain low levels of gluten. For example, a product that contains 16 ppm of gluten could be labeled “gluten-free,” even with traceable levels of gluten. Further, the FDA doesn’t account for oats, which are notoriously contaminated with wheat.
The U.S. labeling guidelines align with the Codex Alimentarius guidelines set by the World Health Organization. Food manufacturers follow the Codex guidelines in the U.K. and European Union. Health Canada also requires products to contain less than 20 ppm to be labeled “gluten-free.”
In contrast, Australia and New Zealand only allow products with no detectable levels of gluten to be labeled “gluten-free.” The countries also provide guidelines for foods containing 20 mg of gluten per 100 grams of food. These products can be labeled “low gluten.”
Why 20 Parts Per Million?
The FDA says it set the 20 ppm gluten threshold based on the following factors:
- There is an unavoidable presence of gluten in foods that carry the gluten-free label.
- It’s the lowest level that can be consistently detected in foods using valid scientific analytical tools.
- Most people with celiac disease can tolerate foods with tiny amounts of gluten.
- The level is consistent with gluten-free thresholds in other countries and international bodies.
Dr. Alessio Fasano, Director of the University of Maryland Center for Celiac Research (the “Center”), played a crucial role in helping the FDA determine the final gluten-free labeling guidelines.
In his book, Gluten Freedom, he details how the FDA used the Center’s landmark study to set the 20 ppm gluten threshold, which is widely accepted by the gluten-free community and food manufacturers today.
He says the Center conducted double-blind studies that measured the intestinal changes in three groups of celiac patients, all of whom were in remission. (Remission is defined as good compliance with the gluten-free diet, no symptoms, and no increased serum autoantibodies.)
One group consumed 0 milligrams (mg) of gluten daily, another group consumed 10 mg, and the third group consumed 50 mg daily. The groups that consumed 0 and 10 mg of daily gluten showed no changes; the group that consumed 50 mg of gluten per day exhibited intestinal injury consistent with celiac disease.
Dr. Fasano shares the following chart in his book to explain further how his team determined the 20 ppm gluten threshold.
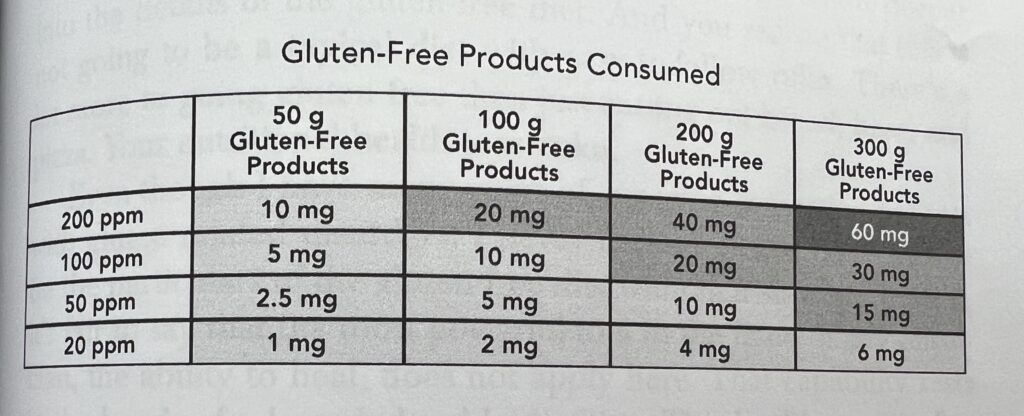
Based on this chart, a person with celiac disease could eat a single product contaminated with 200 ppm of gluten and be safe if they only consumed 10 mg of gluten on the same day.
They also found that a person could consume 300 grams of gluten-free products containing 20 ppm of gluten daily and remain safely below the 10 mg level. Ten milligrams is equal to approximately one-eighth of a teaspoon of flour.
The National Celiac Association offers a great visual of what 10 mg of gluten looks like. The organization says you would have to eat 17 slices of gluten-free bread that contain 20 ppm gluten in order to reach the 10 mg threshold, but you’d only need to eat a tiny crumb of wheat bread (the size of the tip of a pen) to reach that threshold.
What Does 20 ppm of Gluten Look Like?
To visualize what 20 ppm million looks like, think of a sandbox that contains one million pieces of sand. Only 20 pieces of the sand would contain gluten; the rest would be gluten-free.
In the following video, you can see what 20 ppm looks like. The creator extracted 20 pieces of sand from a sandbox containing one million pieces of sand.
Is the 20 ppm Gluten Threshold Enough?
A lot of people in the celiac disease and gluten-free community have questioned if the 20 ppm of gluten threshold is enough, given the following facts:
(1) The current assay measurement is sensitive to a threshold of 5 ppm vs. 20 ppm. This means gluten can be reliably detected in products at levels as low as 5 ppm.
(2) The gluten-free community sees organizations like the GFCO touting that its “certified gluten-free” products contain less than 10 ppm of gluten, lower than the 20 ppm threshold set forth by the FDA.
(3) Home lateral flow devices, like Nima Sensor, can detect gluten levels under 20 ppm, albeit irregularly. (Nima consistently detects gluten above 20 ppm but also often detects gluten under 20 ppm.)
(4) Numerous studies find that adults with celiac disease on a gluten-free diet rarely achieve full mucosal recovery. One study found that only 34 percent of celiac patients achieved mucosal healing after two years.
These are important facts that have caused the gluten-free community to question the 20 ppm gluten threshold and if it needs to be changed given the advancement of technology.
Dr. Fasano wrote in a 2011 letter titled, In Defense of 20 Parts Per Million, why the 20 ppm gluten threshold stands and should continue to stand.
(1) Just because we can measure gluten to the level of 5 ppm, which is a minuscule amount of gluten, it doesn’t mean it’s an effective way to set the threshold, says Dr. Fasano.
Instead, he says, he and his team used scientific methods (remember those double-blind studies and randomized trials?) to establish a safety level for ppms of gluten.
The three-month trial showed that adult celiac patients could safely consume 10 mg of gluten each day without experiencing intestinal damage. Ten milligrams translated into ppms is equivalent to the daily ingestion of more than a pound of gluten-free products containing 20 ppm of gluten.
Dr. Fasano adds, “As far as I know, there are no evidence-based published studies that demonstrate toxicity with exposure to 20 ppm and safety with 5 ppm exposure.”
It’s important to note two flaws of the landmark study that set the 20 ppm gluten threshold. One, the study subjects were only adult celiac disease patients in remission, which meant they were healthy patients with no symptoms or lingering mucosal damage.
Numerous studies reveal that few adults achieve complete mucosal healing. The researchers say nothing about how 10 mg of daily gluten would impact someone struggling to heal the lining of their gut nor how the 20 ppm threshold would impact children.
Furthermore, the study only examined how celiac disease patients reacted to varying levels of daily gluten exposure. People with celiac disease comprise one percent of the population, while 6-7 percent have non-celiac gluten sensitivity (NCGS) or gluten intolerance.
People with NCGS don’t experience intestinal damage consistent with celiac disease. Still, they experience chronic gut inflammation (leaky gut), which can lead to serious disorders such as autoimmune disease, heart disease, and cancer.
The NCGS community currently follows the 20 ppm gluten threshold, but no studies exist to help the community understand if the threshold is safe for them.
(2) According to Dr. Fasano, setting the gluten-free labeling threshold below 20 ppm would likely drastically reduce gluten-free options in the U.S., given factors such as assay variability (margin of testing error).
He adds that thresholds as low as 5 ppm don’t give manufacturers enough flexibility to produce “good-tasting and safe products” and are unnecessarily restrictive. It might lead food manufacturers to no longer create gluten-free products or lower the quality of the products already offered.
(3) Overly-restrictive ppms would force manufacturers to “abide by an unnecessarily restrictive safety threshold” set in the U.S., which may prohibit U.S. companies from competing in the gluten-free global marketplace.
Creating such restrictions, he argues, could complicate and even worsen a celiac patient’s quality of life, which is the opposite outcome of the law’s intent.
While I agree with Dr. Fasano’s argument, it’s important to note that the gluten-free market was valued at $5.9 billion in 2021 and is expected to rise by nearly 10 percent by 2030. The market comprises mostly junk-food brands labeling their foods as “gluten-free” and charging three times as much for the same product.
Most of the gluten-free community (including me) enjoy gluten-free Oreo cookies and Kraft Mac and Cheese options, so Dr. Fasano is right that we don’t want to rock the boat, so to speak. However, putting food manufacturers’ profits over consumers’ health would not be a valid reason for setting the threshold at 20 ppm.
Bottom Line: Is 20 ppm of Gluten Enough?
The FDA’s gluten-free labeling guidelines are enough for most people with celiac disease. Most people consume well below 10 mg of gluten even if they eat multiple products containing less than 20 ppm of gluten each day.
However, how people respond and react to food is bio-individual. Suppose your symptoms persist or your small intestine hasn’t fully healed. You may want to abide by the zero-gluten rule by avoiding packaged foods and never eating out. Did you know that one in three restaurant meals labeled “gluten-free” contained detectable levels of gluten, according to this study?
Zero-gluten is unrealistic and overly restrictive for most people. It would significantly interfere with your ability to travel, participate in social events outside the home, eat various foods, and overall enjoy life.
Therefore, most of the gluten-free community should feel confident that the 20 ppm gluten threshold will keep them safe. Restrictive labeling below the 20 ppm threshold would create unnecessary restrictions for consumers and manufacturers, lower the number of products available to the gluten-free community, and create a new level of food fear and anxiety within the already stressed-out gluten-free community.
What do you think? Please leave a comment to share.
Addendum
Do you need to get tested for celiac disease? I recommend this at-home celiac disease test, which is accurate and reliable because it’s the same test administered by doctors. Be sure to get tested for celiac disease before going on a gluten-free diet – here’s why.
Want to understand gluten-free labeling guidelines better? Read my article, What Gluten-Free Labeling Laws and Certifications Really Mean and Certified Gluten-Free, but Made on Shared Equipment?
Want to learn the ins and outs of living with celiac disease? Read Dear Gluten, It’s Not Me, It’s You and enroll in my Gluten-Free Made Easy 30-Day course that I teach with Dr. Tom O’Bryan, the leading gluten-sensitivity doctor in the world and best-selling author of The Autoimmune Fix.
Learn how to eat out safely in my ebook, The Ultimate Guide to Eating Out Gluten Free.

I have been reading/researching about gluten free options since I was medically diagnosed with Celiac disease in 2011. I thought I was crazy for many years because I kept getting sick eating GF labeled food until I came across an article informing me of the FDA’s 20ppm rule for “gluten free” labeling. Apparently, I am extremely sensitive to gluten (need 0ppm). Now I read ingredient labels very carefully and have had to learn the derivatives of sources, e.g. hydrolyzed protein. I have learned to trust a few brands. I wish the FDA would allow labeling like those in Australia so that the consumers could make a more educated decision about the products they buy. The FDA is not concerned about the ppm level and most likely will not ever change it, unless someone in their family gets sick (i.e. General Mills). The FDA does not care about the consumer, only his/her support of the economy.
I am happy to see you are considering the 20ppm standard. Many maintain that 20ppm threshold is arbitrary and more to do with the limits of testing at the time the rules were promulgated than actual scientific evidence. Are you familiar with a meta study performed by FDA published in 2011 looking at this very issue? It is entitled Health Hazard Assessment for Gluten Exposure in Individuals with Celiac Disease: Determination of Tolerable Daily Intake Levels and Levels of Concern for Gluten? The take away is that for many folks, there really is no safe level of exposure. The authors concluded: ‘The LOC values for gluten in food that correspond with these TDI values at the 90th percentile level of intake
are less than 1 ppm for both morphological (~0.5 ppm) and clinical (~0.02 ppm) adverse
effects. In sum, these findings indicate that a less than 1 ppm level of gluten in foods is
the level of exposure for individuals with CD on a GFD that protects the most sensitive
individuals with CD and thus, also protects the most number of individuals with CD from
experiencing any detrimental health effects from extended to long-term exposure to
gluten.’
I would also like to point out that the FDA rules do not require testing by food manufacturers when labeling a product gluten free. Only when challenged by a complaint is a manufacturer obligated to demonstrate that their product meets the 20 ppm standard.
Finally, I want to touch on the matter of follow-up endoscopy to assess gut healing. I am not sure how many people actually receive this although it is considered the standard of care: a person with an endoscopically confirmed celiac diagnosis is supposed to follow up in six months to gauge the efficacy of the GF diet. In my case, I have been on a dedicated GF diet since Jan 2015 and only recently did I manage to have the follow up procedure. Result? mucosa indicative of celiac disease and villous blunting. While I cannot be sure of the cause of villous blunting in September 2022 – was it the result of some accidental gluten ingestion in the weeks prior – overall I was very please to see that I had villi in the duodenum, albeit blunted.
My point in bringing up my personal experience in relation to the 20 ppm standard is that it is very likely that one can be exposed to gluten at cellularly damaging levels and not have any overt symptoms. I have read that it takes only 3 hours after gluten exposure to register an immunological reaction. And we all know what that means: autoimmune attack leading to potentially systemic inflammation. My concern is that the 20 ppm standard is too high to protect people from the effects of low level chronic gluten exposure. Consider for a moment that the target of the auto-immune response – the enzyme transglutaminase – is found throughout our bodies and not limited to the gut – and you can envision the wide ranging impact of even minute amounts of gluten.
Personally I know that 20ppm isn’t enough for me to not have symptoms.
I appreciate Dr Fasano point of not wanting needless restrictions on consumers or manufacturers. But he also set the standard for treatment for non responsive Celiac disease. The Fasano Diet for non responsive Celiac disease includes no prepackaged foods. (Including prechopped veggies or frozen fruit) due to the risk of gluten contamination. And it has amazing success rate of helping patients go into remission because they are getting glutened from gluten free foods!
There has to be a middle ground between Celiacs continuing to feel sick and having safe and tasty options.
Also how does Australia and New Zealand pull this off, while other countries deem it too restrictive?
Thank you for such great articles! I look forward to your email every Friday.
Look at that chart in the article. You can potentially be safe eating up to 10 mg of gluten each day. Ten milligrams is equal to approximately one-eighth of a teaspoon of flour. Ten milligrams translated into ppms is equivalent to the daily ingestion of more than a pound of gluten-free products containing 20 ppm of gluten.
Does consuming multiple gf products or servings allow gluten to accumulate above that ppm threshold on a daily basis or over time? If so the only safe diet for celiacs is to not consume processed gf foods at all. What’s the thinking on that?