In this article, I share ten facts doctors may not know about celiac disease and gluten sensitivity. This post may contain affiliate links; please read my disclosures.
When faced with a gluten disorder, many people quickly learn that their doctor doesn’t know much about celiac disease, gluten intolerance, and other related gluten disorders, such as autoimmune disease.
It might seem like a doctor should know everything, but they are only human. Most doctors learned little about gluten – and nutrition in general – in medical school, given that U.S. medical schools offer only 19.6 hours of nutrition courses during the average four-year program.
A 2019 study highlighted the poor state of nutrition education in medical schools. Researchers found nutrition knowledge among medical students to be uniformly low despite high interest in nutrition training among medical students.
The researchers say this might be due to the faculty’s lack of nutrition expertise; therefore, nutrition education had not been prioritized for emerging physicians.
Yet, the world needs sound nutrition advice more than ever, especially with the rise of obesity.
According to The World Health Organization, approximately 13 percent of the world’s adult population was obese in 2016. The worldwide prevalence of obesity nearly tripled between 1975 and 2016.
And in the U.S., approximately 42 percent of adults were obese in 2020, and in recent years, the obesity rate increased from 30.5 percent to 41.9 percent, according to the CDC.
Unfortunately, with the rise of obesity comes an increase in chronic diseases, including a surge in preventable diseases such as diabetes and heart disease.
On top of it all, most Americans turn to their doctors for advice about their diet, not realizing how poorly equipped their doctor may be to help them.
Gluten Knowledge Among Doctors is Grim
On top of having little nutrition training, few doctors have studied gluten disorders in earnest. A survey to gauge how much physicians know about celiac disease yielded appalling results.
A questionnaire was given to 1,400 general practitioners, pediatricians, and pediatric and adult gastroenterologists from Europe. On average, the physicians could only answer half of the questions correctly.
Another study in the U.S. showed that only 30 percent of approximately 130 Southern California primary care physicians knew that celiac disease symptoms could begin in adulthood.
I say this not to insult doctors. I believe doctors play an essential role in helping the world research and understand gluten disorders. And some incredible doctors understand gluten’s impact on chronic diseases.
One such doctor, Dr. Yehuda Shoenfeld, published a mind-blowing paper titled “Gluten-Free Diet Can Ameliorate the Symptoms of Non-Celiac Autoimmune Diseases.” The headline says it all.
And Dr. Tom O’Bryan, the leading gluten-sensitivity doctor in the world, explains in his book the critical role gluten plays in chronic disease.
Instead, I say this because I believe anyone suffering from a gluten disorder needs to become more educated than their doctor.
And in a world where people are desperate for sound nutrition advice, it’s unacceptable that doctors don’t have basic nutrition knowledge, let alone any understanding of gluten disorders beyond celiac disease.
In this article, I share ten facts about gluten disorders that most doctors don’t know. This information is meant to inspire the gluten-free community to take matters into their own hands, do their research, and become more knowledgeable than their doctors.
Fact #1: Celiac disease and gluten sensitivity are not exclusively gastrointestinal (GI) disorders
Unfortunately, most doctors won’t test someone for celiac disease or gluten sensitivity without gastrointestinal symptoms such as chronic bloating, gas, diarrhea, constipation, or stomach aches.
However, only some celiac disease and gluten-intolerant patients experience GI issues. Instead, celiac disease often manifests itself through many non-GI symptoms, including brain disorders, dental and mouth disorders, failure to thrive or delayed puberty, autoimmune diseases, anemia, nutrient deficiencies, chronic fatigue, osteoporosis, joint pain, and more.
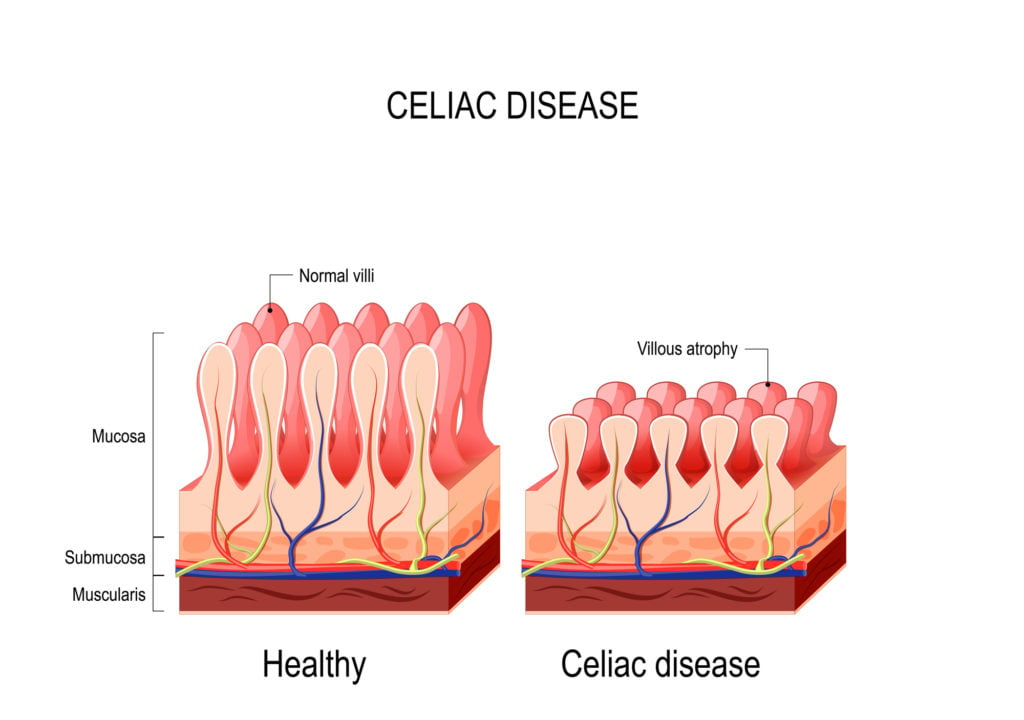
Fact #2: Partial villous atrophy may be a sign of early celiac disease
Partial villous atrophy or gut inflammation can mean a person has (or will soon have) celiac disease; it can also be a sign of gluten sensitivity.
However, most doctors won’t give an official celiac disease diagnosis unless they see total villous atrophy.
The villi are the hair-like follicles surrounding the small intestine responsible for absorbing and distributing nutrients from the food to the rest of the body. In people with celiac disease, the villi are flattened and damaged.
Even if a doctor discovers that the villi surrounding the small intestine are partially damaged, a doctor won’t diagnose celiac disease or tell their patient to go on a gluten-free diet since the diagnosis calls for “total” villous atrophy.
The truth is partial villous atrophy is likely an early sign of celiac disease, and prescribing a gluten-free diet at the sign of partial villous atrophy could potentially deter full-blown disease.
Fact #3: Gluten sensitivities are just as severe as celiac disease
Many gluten-intolerant people have told me their doctors say they don’t have to be “strict” about their gluten-free diet since they don’t have celiac disease.
This has led some people with gluten sensitivity to be more relaxed in following a gluten-free diet, perhaps eating foods prepared in a shared fryer (known as gluten cross-contamination) or eating oats, whether labeled gluten-free or not.
Sadly, such misinformation is why people with gluten sensitivities are often more chronically sick than people with celiac disease.
In fact, a person with gluten sensitivity has a 72 percent higher chance of early death than someone with celiac disease, according to a study published in the Journal of American Medicine.
This discrepancy in mortality risk is likely because someone with celiac disease actively manages their disorder by adhering to a strict gluten-free diet.
In contrast, people with just gluten intolerance are not as strict in their dietary vigilance and may not have achieved symptom resolution.
Fact #4: Patients can’t outgrow celiac disease or gluten sensitivity
Several former gluten-free people have started eating gluten again because their doctors told them they were miraculously cured.
Long ago, before celiac disease was understood as it is today, parents would send their children with distended bellies to a clinic in California to be treated for celiac disease.
The children were fed bananas along with meat, cheese, and vegetables. After six months, when the babies were better, they were sent home and told they were “cured” of celiac disease.
We now understand that they weren’t cured at all and that it wasn’t bananas that made the babies better; instead, it was the fact that the babies avoided gluten that helped them improve.
As the banana babies grew up, many went on to deal with a slew of maladies throughout their lives. And once someone goes back on gluten, the cycle of damage starts over again, often with a vengeance. (See Does Gluten Intolerance Increase After a Gluten-Free Diet?)
The same is true in non-celiac gluten-sensitive patients because, as Dr. Tom O’Bryan says, gluten sensitivity is permanent. The body produces memory B cells that remember gluten and produce antibodies to gluten every time someone eats the sticky protein.
Fact #5: Someone may have an issue with gluten despite a negative celiac test
If a celiac disease blood test is negative, it doesn’t mean the person doesn’t have an issue with gluten.
In fact, 18 million people in the U.S. don’t have celiac disease; instead, they have an issue with gluten – or, more likely, wheat. One in seven people has a wheat-related disorder.
Gluten sensitivity testing has come a long way, and it’s vital that someone who suspects a wheat-related disorder undergo an elimination diet to determine if they can – or can’t – tolerate gluten.
Also, several blood tests, including Cyrex Array 3x and Wheat Zoomer, can check if the immune system produces antibodies to various wheat peptides, including gluten and non-gluten components.
Fact #6: Don’t go gluten-free until celiac disease has been ruled out first
Well-intentioned doctors often tell their patients to remove gluten from their diet to “see how they feel.” However, these doctors fail to first test their patients for celiac disease.
When the patient feels better after removing gluten and then demands to know if they have celiac disease, they are usually saddened to learn that they must return to eating gluten.
They have to do what is called the Gluten Challenge to get an accurate celiac disease diagnosis since a person must eat gluten to get an accurate result. This can be a difficult, if not impossible, task as many people have lost their tolerance for gluten and suffer immensely as a result.
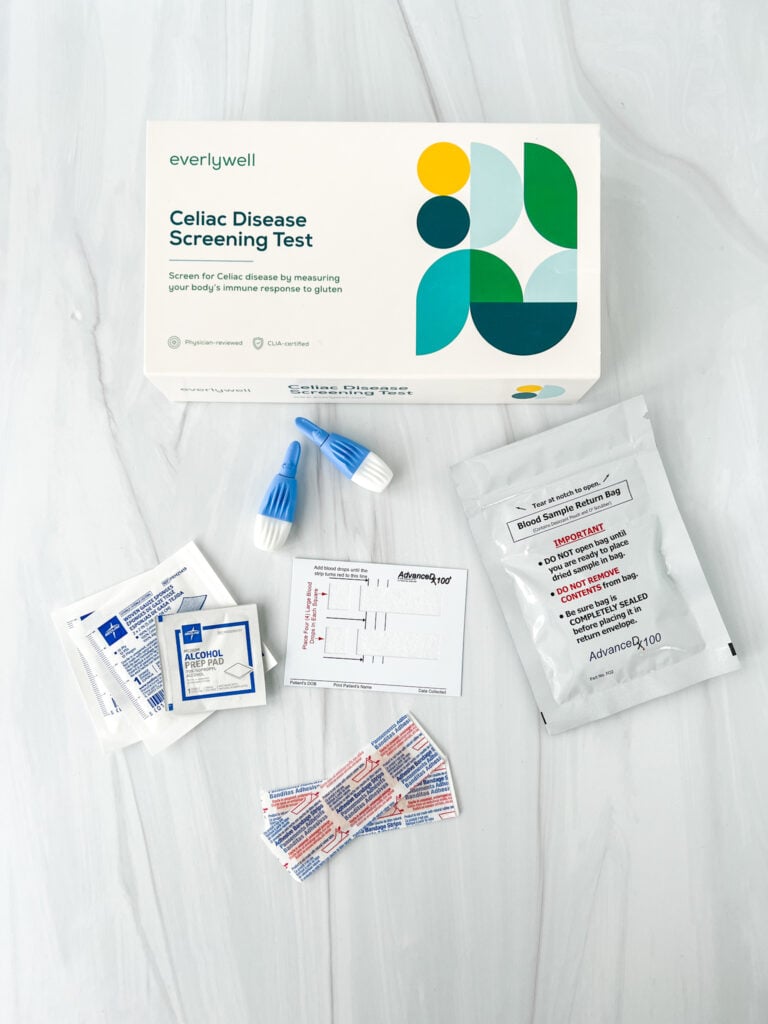
Before recommending a gluten-free diet, doctors must first test their patients for celiac disease. If a doctor doesn’t – or won’t – administer a celiac disease, I recommend ordering an at-home celiac disease test first.
I believe ruling out celiac disease should be the first step in determining if someone has an issue with gluten for various reasons, which I detail in this article.
Fact #7: Doctors know little about the microbiome
The great Hippocrates, the father of modern medicine, once said, “All disease begins in the gut.” Yet, few doctors look at the gut as the root cause of chronic disease, despite a large proportion of the immune system residing in the GI tract.
People have more bacteria in their guts than cells in their bodies, and these bacteria make up what is known as the gut microbiome.
It’s why taking care of the gut, and ensuring bad bacteria don’t take over, is part of maintaining an overall healthy immune system and keeping chronic illness at bay.
The adage, “You are what you eat,” rings more true today than ever. This is why doctors need to prescribe gut-healing foods and probiotics over medications when managing chronic diseases.
Most medications only mask symptoms vs. address the root cause. For example, PPIs prescribed to treat heartburn and acid reflux may relieve a person’s symptoms, at least at first, but over time, such medications will likely cause leaky gut and a slew of symptoms related to poor gut health.
Fact #8: There is more to healing from celiac disease than a gluten-free diet
Many doctors, including mine, tell their newly diagnosed celiac patients to go gluten-free to feel better. And while the gluten-free diet is a necessary treatment protocol for those with celiac disease, it’s only scratching the surface of what needs to be done to heal one’s body. While necessary, removing the irritant food (gluten) isn’t enough.
The gluten-free diet is only the first step in a long line of changes needed to heal from celiac disease. Learn more about how I healed my body and put my symptoms into remission in my book, Dear Gluten, It’s Not Me, It’s You.
If you’re struggling to go gluten-free and want more professional guidance from a nutritionist specializing in celiac disease and gluten intolerance, consider enrolling in my SIGNATURE Gluten-Free Course.
Fact #9: The actual prevalence of celiac disease may be triple, and it’s on the rise
It’s widely accepted in the medical community that 1 in 133 people, or 1 percent of the American population, has celiac disease, according to Dr. Alessio Fasano, a leading celiac disease researcher.
Because celiac doesn’t affect a larger number of the population, many doctors don’t think to screen for it, especially in children who don’t exhibit classic GI symptoms.
However, emerging evidence suggests that celiac disease prevalence might be triple the rate than initially thought.
Dr. Edwin Liu, Director of the Colorado Center for Celiac Disease, studied 1,339 children born in Denver, CO, from 1993-2004. Of the 1,339 study participants, 112 developed celiac disease. Thirty percent of the children diagnosed with celiac disease were considered asymptomatic.
He found the prevalence of celiac disease (by age 15) to be 3.1 percent, triple the rate previously found by Dr. Fasano’s original research.
Furthermore, Dr. Liu’s study suggests that there may be an “upward trend of celiac disease occurrence” in this new generation of children. In fact, Dr. Liu found the rate of occurrence was 1.6 percent for study participants at age five, but it had doubled to 3.1 percent by age 15.
Because celiac disease affects a larger percentage of the population than first thought, and research indicates an “upward trend” in its occurrence, doctors must screen for celiac disease in children with both GI and non-GI symptoms.
Fact #10: Non-celiac gluten sensitivity needs a place at the table
It’s no secret that celiac disease is a known disorder; however, little is known about non-celiac gluten sensitivity. This has led many doctors to question if gluten sensitivity is a “real” disorder.
It’s important to note that just because there isn’t much research related to gluten intolerance, it doesn’t mean the disorder isn’t real. Never mistake lack of research with lack of disorder.
The good news is that the research is finally catching up to what millions of people already know and experience, even if their doctors think gluten intolerance is just a passing fad.
Columbia University Medical Center researchers set out to gauge if non-celiac wheat sensitivity is a real condition. They took intestinal biopsies of 160 patients. Of those 160 subjects, 80 had self-reported non-celiac wheat sensitivity, 40 had celiac disease, and 40 had neither condition.
The researchers found that individuals with non-celiac wheat sensitivity experienced higher levels of intestinal permeability – aka, leaky gut – than healthy subjects. Prior research has also shown that gliadin, a component of gluten, increases intestinal permeability.
The researchers also found that the non-celiac wheat sensitivity participants experienced a chronic inflammatory response resulting from the bacteria and other microbes from the gut leaking into the bloodstream, as well as epithelial cell damage similar to the damage found in people with celiac disease.
Furthermore, the researchers found that once the non-celiac wheat-sensitive individuals went on a gluten-free diet, their inflammation and cell damage markers improved significantly after six months.
These emerging studies demonstrate that gluten sensitivity is real, and it’s time that the medical community sees gluten intolerance as a serious, treatable disorder.
Find a Gluten-Free Practitioner
I’m a trained Certified Gluten-Free Practitioner, meaning I have been trained to understand all gluten disorders and can help my clients advocate for the tests and nutritional interventions they need.
Please consider hiring me for 1-to-1 celiac nutrition coaching if you need help beyond going gluten-free.
If you’re still struggling with the gluten-free diet, I highly recommend enrolling in my SIGNATURE Gluten-Free Course.
Additional Reading
- Do You Have Gluten Intolerance? How to Test for Non-Celiac Gluten Sensitivity
- What to Expect When Getting Tested for Celiac Disease (Blood Test and Endoscopy)
- Supplements for Celiac Disease and Gluten Intolerance
- Beginners Guide to Gluten Free
- Can Celiac Disease Kill You?
- 12+ Must Read Books about Celiac Disease and Gluten-Free Living
- What is Silent Celiac Disease?
I was first diagnosed with Celiac disease at age 68. I had previously been diagnosed with osteopenia several years earlier. No physician had ever suspected Celiac disease until I went to a rheumatologist at a large teaching hospital. She had background in dietary/nutrition, which was one reason I selected her off the internet. Got a referral from my GP. The rheumatologist had me complete an 8 page questionnaire on diet/ medications/ exercise/vitamin D exposure. She reviewed my dexascan reports. Finally, she did the blood test for Celiac disease and aTTG was elevated at 88. Confirmed Celiac with intestinal biopsy. Bingo!! Puzzle solved. After a year on the Gluten free diet, aTTG was greatly reduced to 23. Thank God I found this doctor! The diet has been a lifestyle changer, but so essential for my health.
Very good information, thx , I to am gluten free and soy free and I need grass fed and organic meats and organic eggs etc. it’s getting better though the years go by I’ve been like this for 10 years. I have a new Dr. and just had a visit with her and she had know idea how bad gluten is to the body and meats she was very surprised. I gave her a lesson lol. She apparently was glad I gave her information,thx again Cindy from Colorado
Thanks Debbie. Glad you’re feeling better!
I have been diagnosed with severe celiac disease and have been on a GF diet for a few months now..feeling much better..fingernails slow in growing back..! enjoying the articles,etc!!
Thank you Pauline. You can subscribe to our newsletter here https://www.goodforyouglutenfree.com/sign-up-for-our-newsletter/
I have celiac and have really enjoyed reading these articles. I would like to sign on to your blog
Hi Jenny,
Your blog is a wealth of information – thank you! There are now many direct-to-consumer lab tests available that can be ordered online – no doctor visit required (including the Array 3 test by Cyrex Labs that you mention above). You simply order and pay for the lab test online, choose the blood draw lab/location most convenient to you, print the order and have the test at your local lab. Results are then available for you to view online or via email.
I order my own blood tests to monitor my thyroid numbers (also because most conventional endocrinologists will not order the full range of blood tests for you) and also to monitor my HA1c numbers (to be certain my blood glucose levels are good and that I am not at risk for type 2 diabetes – my numbers were elevated prior to going gluten-free and I was able to bring them down into a good range within several months) and also to monitor my nutrient levels (many which were off and not adequate due to years of undiagnosed gluten sensitivity, but I was able to correct after going gluten-free and taking supplements).
Both of these sites offer the Cyrex tests (I’m sure there are others as well):
https://www.truehealthlabs.com/searchresults.asp?Submit=Go&Search=cyrex
https://mylabsforlife.com/lab-test/array-3-wheat-gluten-autoimmunity-reactivity-profile-cyrex-laboratory/
Hi Margaret. Yes celiac genes can turn on later in life, and and intolerance can develop later in life too. It’s very common. Feel well!
Is it possible to develop Celiac or gluten intolerance at the age of 58. I going to do as you recommend and get the tests. I feel horrible!! You are wonderful and so informative. I’m so blessed to have your blog!!
Sincerely,
Margaret Adamson
I have removed that information from the post because, as I said in the post, I cannot independently verify this information even though someone said it (that just makes it anecdotal though). Until I can learn more about this, I have deleted the paragraph you have referenced. Thank you for taking the time to comment.
Canadian medical insurance most certainly does cover endoscopies! I reported anemia (only) to Gastroenterogist when registering for a colonoscopy (also covered). He ordered the blood test immediately (positive), then called back to advise of those results and to say he would be adding the endoscopy when I had my colonoscopy. Please update your article as it is incorrect.