
Celiac disease and gluten intolerance (non-celiac gluten sensitivity) are different disorders with similar symptoms and treatment options. This post contains affiliate links and information you should discuss with your healthcare provider. Please see my disclosures.
Millions of people in the U.S. and worldwide avoid gluten, a protein found in wheat, barley, rye, and derivatives of these grains, due to celiac disease or because they innately feel like gluten is making and keeping them sick.
With the spotlight on gluten, you might wonder if gluten might be behind your fill-in-the-blank ailment(s).
Reliable studies show that all humans experience an inflammatory response to gluten. While this doesn’t mean everyone has an issue with gluten, it suggests that gluten could be the root cause of other diseases.
Unfortunately, 60 percent of American adults live with at least one chronic condition, and 42 percent have more than one. These diseases bring high emotional and physical costs and put unsustainable financial burdens on the private and public sectors. Most of these adults don’t know the root cause of their suffering.
In my years of studying nutrition, I’ve realized that what you eat indisputably affects how you feel. Food can be used as a tool to heal or hurt our bodies. “Food is medicine,” the great Hippocrates, father of modern medicine, once said.
And while the gluten-free diet has been made to look like a “fad” diet by celebrities or those trying to eat a certain way to “fit in,” for those with serious gluten disorders, like celiac disease and gluten intolerance, it’s far from a fad for them.
No one eats gluten-free long-term because they want to or because it’s “fun.” They do it because they want to feel better. No one wants to pay more money, eat less-delicious food (at times), or feel like a social pariah just for the bragging rights to say they’re on a gluten-free diet.
You may question your relationship status with gluten if you’re experiencing chronic inflammation or pain. But before you say goodbye to gluten, let’s first understand celiac disease vs. gluten intolerance and what may be affecting – or afflicting – you.
My award-winning book, Dear Gluten, It’s Not Me, It’s You, chronicles my journey to break up with gluten and heal my body in the aftermath.
What is Celiac Disease?
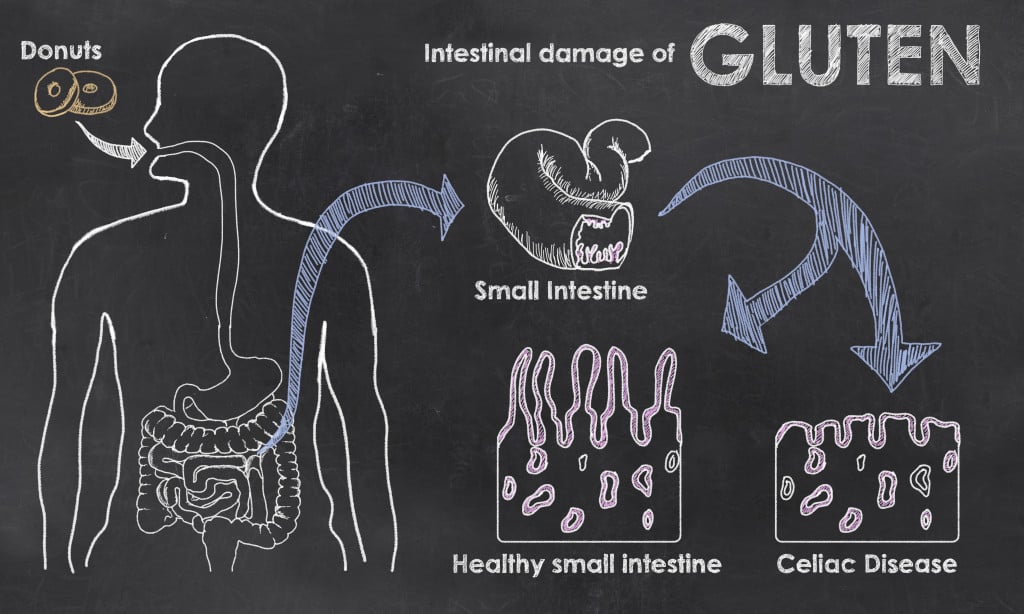
Celiac disease is an autoimmune disease signaled by an immune system attack on the small intestine.
Whenever someone with celiac disease eats gluten (the trigger food), white blood cells produce antibodies that mistakenly attack the small intestine’s lining, resulting in intestinal damage and villous atrophy.
The small intestine is a 20-25 foot tube lined with microvilli. These villi are finger-like follicles surrounding the small intestine and look like shag carpet.
The microvilli surrounding the small intestine are completely worn down in someone with celiac disease. It looks like a smooth, flat surface rather than finger-like flowing follicles.
The small intestine is essential to your digestive system and overall well-being. It’s responsible for helping you absorb nutrients from your food, and then it helps to distribute those nutrients to every cell in your body.
With a malfunctioning or damaged small intestine, people with celiac disease are nutrient often deprived and experience a slew of related symptoms such as fatigue, anemia, infertility, low bone density, dental and oral issues such as canker sores and geographic tongue, mental disorders, skin rashes, failure to thrive, and more.
How Many People Have Celiac Disease?
According to Dr. Alessio Fasano, one of the world’s leading celiac disease researchers, about 1 in 100 people, or 1 percent of the U.S. population, has celiac disease.
This puts celiac disease as humankind’s most prevalent genetically-linked disease, occurring much more frequently than type 1 diabetes, cystic fibrosis, or Crohn’s disease, according to Dr. Fasano in his book, Gluten Freedom.
Dr. Fasano says that celiac disease is caused by a combination of three factors – each of which must be present for celiac disease to thrive:
- Genetic predisposition
- Consumption of the trigger food (gluten)
- Intestinal permeability
There is no cure for celiac disease nor any approved treatment options beyond the gluten-free diet, even though celiac disease is the most researched autoimmune disease in the world and the only autoimmune disease in which the environmental trigger (gluten) has been identified.
What is Gluten Intolerance?
Gluten intolerance, also known as non-celiac gluten sensitivity, has only started to be recognized as a real medical disorder. Unfortunately, the medical community doesn’t always take gluten intolerance seriously despite millions of people testifying that avoiding gluten makes them feel better.
Many more people experience gluten intolerance than celiac disease. According to Beyond Celiac, gluten sensitivity affects 18 million people or six percent of the U.S. population. In other words, gluten intolerance affects six times as many people as celiac disease!
On top of that, there is a lot of confusing information about how to classify gluten intolerance (if it’s not an autoimmune disease, what is it?) and a lot of controversy about how to diagnose and treat it.
Gluten-intolerant people experience an inflammatory response every time they consume the gluten protein.
Unlike people with celiac disease who experience villous atrophy, they experience intestinal inflammation.
While gluten intolerance is considered a gluten-related disorder, it’s not classified as an autoimmune disease (yet), even though people with gluten intolerance often develop and experience the same roaring symptoms as those with celiac disease when exposed to gluten. If unmanaged, gluten intolerance may lead to the same chronic symptoms and damaging conditions as someone with celiac disease.
Celiac Disease vs. Gluten Intolerance
Now that I’ve explained the basics of celiac disease vs. gluten intolerance, I want to outline the main differences and similarities between the two disorders.
(1) Number of people affected
Only about 1 percent of the U.S. population has celiac disease, while a much more significant percentage of people, about six percent, have non-celiac gluten sensitivity.
(2) Symptoms
Exposure to gluten in both celiac disease and gluten intolerant patients can result in similar symptoms, including but not limited to gastrointestinal disorders, skin conditions, bone, joint, and muscle pain, nutritional deficiencies, mental health disorders, and oral or dental diseases.
(3) Testing
Doctors utilize a simple blood test for celiac disease. The test looks for specific gluten antibodies. Doctors can order the test, or you can order this at-home celiac disease test to do the test in the privacy of your own home. When doing an at-home test, it’s important to discuss the results with your doctor.
Unlike celiac disease, there are no approved bio-markers for testing for gluten sensitivity, and there is no widely-accepted blood test.
Instead, the current guidelines recommend a 4-6 week elimination diet as the gold standard for diagnosing non-celiac gluten sensitivity. Read, Do You Have Gluten Intolerance? How to Test for Non-Celiac Gluten Sensitivity, to learn more about how to get “tested” for gluten intolerance and what an elimination diet entails.
While the guidelines recommend an elimination diet for diagnosing gluten sensitivity, there are also a few blood tests to consider.
Leading gluten sensitivity expert Dr. Tom O’Bryan, author of The Autoimmune Fix, recommends testing for gluten sensitivity using a Cyrex Labs Array 3x or Wheat Zoomer test. These tests examine a variety of gluten peptides that may indicate your body’s distaste for gluten.
Unfortunately, few insurance companies will cover the costs associated with these tests, given that they are not (yet) a widely accepted way of diagnosing gluten sensitivity.
(4) Immune response
Celiac disease and gluten intolerance cause different immune system responses.
People with non-celiac gluten sensitivities tap into the body’s innate (nonspecific) immune system. Innate immunity is the body’s first defense against foreign invaders that want to attack your cells, such as viruses, bacteria, and parasites.
Your innate immunity occurs naturally, as it’s “innate.” For a pathogen to attack your cells, it will have to get past your innate immune response first.
On the other hand, people with celiac disease experience an adaptive (or acquired) immune system response to gluten over time.
Adaptive immunity is your body’s second line of defense against invaders and is much more complex.
Once an invader (gluten) is introduced into the body, the adaptive immune system creates an army of immune cells designed to attack that specific antigen. The immune system remembers those antigens to initiate future attacks more efficiently.
(5) Damage caused
People with celiac disease experience damaged and flattened microvilli (villous atrophy), while people with gluten intolerances typically have normal but inflamed villi.
(6) Mortality rates
A 2009 study published in the Journal of the American Medical Association (JAMA) aimed to understand mortality rates associated with gluten disorders. This is the largest study ever published on this topic.
Researchers examined 351,000 intestinal lining biopsies and found 46,121 patients on the “celiac spectrum.” Specifically, researchers found:
- 29,096 had celiac disease (with damaged microvilli)
- 17,025 showed early stages of celiac disease development (the microvilli were showing early signs of being damaged)
- 13,000 did not have worn-down microvilli or positive blood work, yet they had gluten sensitivity and inflammation
Researchers found that people with celiac disease had a 39 percent increased risk of early mortality; however, even more shocking is that people with inflammation due to gluten sensitivity had a 72 percent increased risk of premature mortality!
In other words, someone with gluten sensitivity has a higher risk of early death than someone with celiac disease. If this isn’t a good enough reason to take gluten intolerance seriously, I don’t know what is!
(7) Prevalence of other diseases
Research indicates that 25 percent of patients with autoimmune diseases tend to develop other autoimmune disorders.
Because celiac disease is an autoimmune disease, people with celiac disease may have a higher risk of collecting other autoimmune diseases than someone with gluten sensitivity.
However, it’s important to note that many researchers say gluten sensitivity is a precursor to autoimmune disease, and Dr. O’Bryan makes a clear argument for this in his book. This means both disorders, if left unmanaged, put someone at higher risk for accumulating additional autoimmune diseases.
What Do You Have?
You must talk to your doctor if you suspect you have an issue with gluten or take an at-home celiac disease test, then speak to your doctor about the results. You’ll want to rule out celiac disease first and foremost. To be accurate, you must be eating gluten for a celiac disease test, so don’t implement a gluten-free diet before ruling out celiac disease first. Read my article, STOP! Don’t Go Gluten-Free Until You Read This.
If you’ve already eliminated gluten, you may consider taking the Gluten Challenge, where you reintroduce gluten to your diet for a short period and then get tested for celiac.
If the celiac test is positive, you have celiac disease, and your doctor will likely follow up on your diagnosis with an endoscopy procedure to biopsy the small intestine.
If there is no evidence of celiac disease (e.g., a negative blood test), but you still have an inflammatory reaction when you eat gluten, you likely suffer from gluten intolerance. At this point, you’ll want to work with a health professional to implement an elimination diet.
If you find out after testing and an elimination diet that gluten isn’t the issue, talk to your doctor about if something more may be at play, like candida, SIBO, h.pylori, IBS, or a different digestive disorder. Not everything can be blamed on gluten.
Such an incredible story. The power of food is real! Glad you’re doing much better.
I’m a 71-year-old woman who is active and loves to walk my dogs a couple of miles a day in the woods. In the last few years, I’ve been experiencing arthritis in my feet and hands. Recently, I have been having terrible pain in my hips; I could hardly walk, and sleeping on either side was painful. I was worried I was going to have to get both hips replaced. I had wondered about gluten in the past, so I decided to cut it out of my diet. Practically the next day, I had no more pain in my hips while awake or sleeping. I couldn’t believe it! I am very gluten-intolerant and am doing my best to be gluten-free now.
Tested negative for Celiac, but genetic testing shows positive for 1 of the 2 main genes common in those with Celiac. Lifetime of gut issues (I am 65). Just started gluten free clean eating, along with a quality probiotic. I feel better. I did, however, choose to eat a sandwich made of regular white bread. BIG MISTAKE!! Within 30 minutes, severe abdominal bloating and pain, followed by several bouts of painful diarrhea. That was 4 days ago. Bone broth is helping.
recently diagnosed with celiac disease, eating non gluten food, in two months I have felt much better. I read all I can about this so I can remain ok feeling. Thank you for your articles!!
Great info. I’m starting the testing with upper & lower G.I. I’ve had digestive problems for 30 + yrs. Have jerked body about with vegetarian eating, Dr. Atkins since 1975, off & on. Plus other weird eating. Finally beginning to understand digestive problems with your help. Going to get gut healthy even if it kills me. teehee. Thankx, Kathleen
Do you mean your celiac test was negative? I think if you continue to get negative tests but you know gluten makes you sick, avoid it. You don’t need a diagnosis to know how your body reacts to certain foods. Gluten can be tied to other conditions (skin and thyroid) although the research isn’t there yet. Don’t mistake lack of research with a nonexistent condition though. Gluten sensitivity is real! Feel better friend.
I had the blood test done for gluten but it was negative. And I know I’m sensitive to gluten.So what other tests can I take to make sure .I also am hypothyroidism.Gluten is a big culprit for people who have hypothyroidism.
I was itchy for two months and was wandering if it was gluten ?
The treatment for celiac is the same as a gluten sensitivity. Just the way gluten affects your body is different. You can have celiac and sensitivity and wheat allergy. And you can just have one. Does that make sense? Please keep in mind you can’t be allergic to gluten. You can be allergic to wheat though.
Hi Jenny, I appreciated your article – thank you! I have read many articles on the difference between gluten intolerance and celiac disease, but the one question I never see answered is this: since I was diagnosed as allergic to gluten with a blood test, does this mean I have celiac disease? If not, apparently there are at least 3 options: gluten intolerance, gluten allergy, or celiac disease. Is that right? Since I know I’m allergic to gluten, I just don’t allow it in my diet, so it makes little difference if I have celiac or not – I just assume so to be safe – but I would like to better understand. Thanks! Stacy
Thank you! You have wrote do many great things, and all the recipes make me do hsppy!! Thank you!!!
Hi Cara obviously this is a deeply personal decision but if gluten makes you sick, I would not go back on it just to get a diagnosis where the outcome and treatment is the same. If there is ever a cure and you need a diagnosis, you can make that decision to eat gluten again in order to get tested. Good luck.
Thank you for your articles. I have been struggling for a while now with my diet. A couple of years ago finally narrowed down that gluten was the problem. Unfortunately, I had no idea that there was such a thing as Celiac or gluten intolerance. I just cut out the thing that was making me soooooo sick.
I’ve been gluten free for about 2 years and never tested. I know it’s to late to get tested because it could come up with a false negative.
Should I just keep on my gluten free life style and not worry about being tested now?
Thank you for your comment Brenda. I’m glad I could help you. Be well!
Thank You Jenny for all of this very valuable information regarding celiac disease and gluten intolerance. Recently disgnosed with celiac disease, (last week) I’m in the “why” and information gathering stage. I have a lot to learn and from here on out, will look at food and my diet very differently. Brenda