
Three factors cause celiac disease, and in this post, I’ll share these three factors and discuss if celiac disease is preventable. This post contains affiliate links. Please read my disclosures.
A celiac disease diagnosis can turn a person’s life upside-down. Celiac disease is an autoimmune disease where the body’s immune system mistakenly attacks the healthy tissue surrounding the small intestine whenever a person with celiac eats gluten. Currently, there is no cure for celiac disease, nor are there treatment options beyond a strict, lifelong gluten-free diet.
Gluten is a protein found in wheat, rye, barley, and sometimes oats, and it’s hidden in many common foods. People with celiac disease must be careful not only to avoid foods that contain gluten but also to avoid foods that may have come in contact with gluten during the manufacturing or preparation processes. This is known as gluten cross-contamination.
The gluten-free diet is burdensome and can reduce the quality of one’s life. The emotional burden of the gluten-free diet is most often felt when eating at restaurants and traveling where the risk of gluten cross-contamination is high.
Understanding what causes celiac disease and the factors that lead to diagnosis may hold clues in whether or not celiac disease is preventable.
What Causes Celiac Disease?
Celiac disease is a genetic disorder, and researchers say that 99 percent of people with the disorder carry one of two genes, HLA-DQ2 or DQ8. This simple at-home celiac genetic test can help a person determine if they carry one of the celiac genes.
Knowing if a person has one of the celiac disease genes will not only help them determine if they might get celiac disease one day but also might help them prevent the genes from ever turning on or activating.
Of note, 35-40 percent of the American population carry one of the celiac genes, yet only 2-3 percent of people with the genes ever go on to get diagnosed with celiac. This means only a small fraction of celiac gene carriers actually get celiac disease. Why?
In The Autoimmune Fix by Dr. Tom O’Bryan, Dr. O’Bryan says that while genes make a person genetically vulnerable to a disease, they do not dictate whether or not that person will eventually get that disease.
In fact, he and other experts say that three factors must be present in order for someone to get diagnosed with celiac disease.
Factor #1: Genes
In order to have celiac disease, a person must carry one of the two celiac genes – HLA-DQ2 or DQ8. A person inherits these genes from one or both of their parents, which means celiac disease can run in families, with first-degree relatives (siblings, parents, children) being at the highest risk.
Again, having HLA-DQ2 or DQ8 genes means that a person has a genetic predisposition to celiac disease; it doesn’t mean he or she has or eventually will have celiac disease.
Factor #2: Gluten
Celiac disease is triggered by gluten. Therefore, a person must consume gluten for the celiac disease genes to be activated. Celiac disease is the only autoimmune disease in the world in which the trigger (gluten) is known.
A simple blood test is used to determine if a person has celiac disease; however, for a celiac disease blood test to be accurate, a person must eat gluten. Without the presence of gluten, a blood test cannot determine if a person is making antibodies to gluten. This is why it’s extremely important for someone to get tested for celiac disease before implementing a gluten-free diet.
Factor #3: Intestinal Permeability (aka, Leaky Gut)
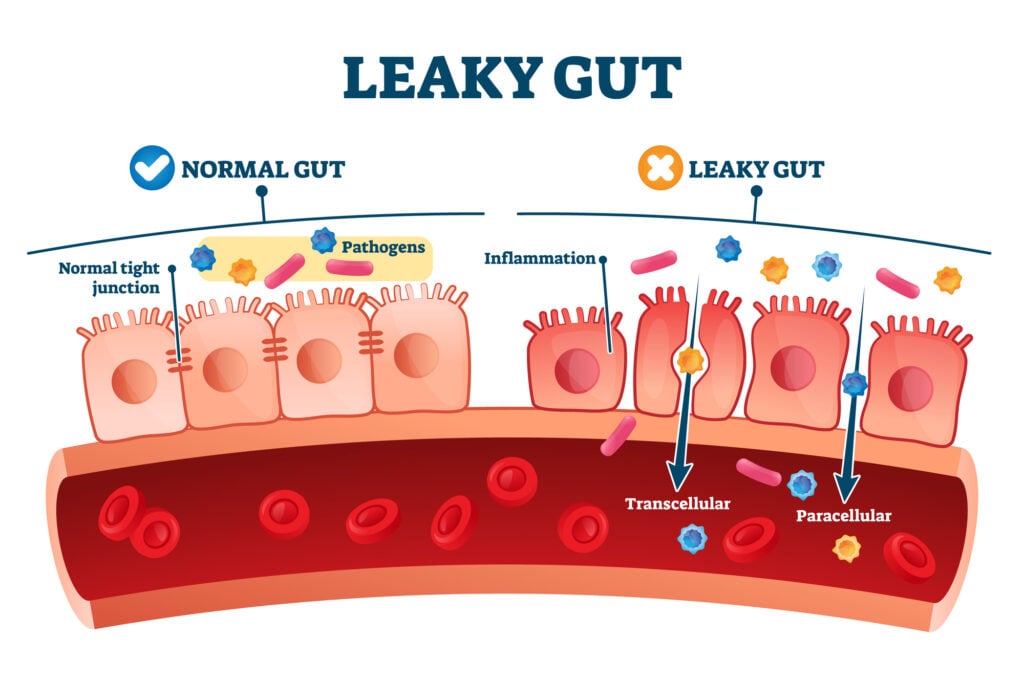
The third factor that causes the celiac disease genes to activate is intestinal permeability, also known as leaky gut. When a person has poor gut health or experiences some health episode that affects their gut flora, their body becomes ripe for disease.
Unfortunately, intestinal permeability can occur anytime and is often triggered by undiagnosed food sensitivities, trauma, stress, environmental toxins, pregnancy, viruses, and other external factors.
Gluten also can lead to intestinal permeability and contribute to the cycle of poor gut health. Gluten is a difficult protein for people to digest. When undigested gluten particles break through the paper-thin intestinal lining and enter the bloodstream, they not only create intestinal damage but also inflammation in the body.
Is Celiac Disease Preventable?
While a person cannot control whether or not they have one of the celiac disease genes, they may be able to take some preventive steps to deter the celiac genes from ever turning on, including:
(1) Follow a Gluten-Free Diet
Following a proactive gluten-free diet may deter the celiac disease genes from turning on and potentially deter gluten-induced damage to the gut.
It’s much easier to follow a preemptive gluten-free diet (without celiac disease) than a strict gluten-free diet (with celiac disease).
In fact, people with celiac disease have to be extremely careful about any food that crosses their lips. However, someone on a proactive gluten-free diet (without celiac) can be a bit more relaxed about eating out and traveling. While they avoid gluten, they won’t experience the same intestinal damage and [sometimes] painful symptoms that someone with celiac disease experiences when they inadvertently eat small amounts of gluten.
Please note that many healthcare professionals don’t recommend avoiding gluten without celiac disease or non-celiac gluten sensitivity; however, the truth is most people can live full and healthy lives without gluten, and the science on gluten disorders is becoming clearer by the day.
In fact, a 2022 study by Dr. Yehuda Shoenfeld found that a gluten-free diet can significantly reduce symptoms associated with non-celiac autoimmune diseases in most autoimmune sufferers.
When following a pre-emptive gluten-free diet, a person should eat plenty of gluten-free whole grains and fiber-rich foods, take some supplements to maintain healthy nutrient levels, and avoid these dangers associated with the gluten-free diet.
(2) Employ Good Gut Health
It’s always wise to maintain good gut health as changes in the gut can lead to intestinal permeability and ultimately affect gene expression.
Those worried about getting celiac disease should eat a diet rich in anti-inflammatory foods, take gut-boosting supplements and probiotics, avoid antibiotics unless absolutely necessary, and avoid stress because stress can adversely alter the microbiome.
Again, such healthy behaviors may only deter celiac genes from turning on, but no diet or lifestyle is foolproof, and many environmental toxins and triggers beyond one’s control can impact gut health and gene expression.
Additional Reading
Enjoyed this article? Also, read these articles:
- 5 Dangers Associated with the Gluten-Free Diet
- Dear Gluten, It’s Not Me, It’s You (book)
- Celiac Disease in Babies
- Genetic Testing for Celiac Disease
- How to Get Tested for Celiac Disease
- 10 Signs and Symptoms of Celiac Disease
- 10 Facts Your Doctor Doesn’t Know about Celiac Disease
- 10 Signs of Celiac Disease in Kids
- The Emotional Burden of the Gluten-Free Diet
We are having our 4 year-old tested for celiac disease later this week. If he does have it, this article shed light on how it could have developed. He had an ear infection every other month as a baby, which included the time period he started eating bread. Antibiotics would have had a great effect on his gut microbiome thus allowing the trifecta to occur for him.
Thank you so much for the feedback!
That is a great point Jim. Our thoughts control much of how our genes express themselves. Thank you for adding that idea to the mix!
Great work, Jenny. Well said and clear. My work is in the world we tend to label as “thinking and imagination” that addresses the possibility to turn genes on and off by certain levels of thinking – epegenetics and how we do that. Epignetics needs real researchers as well.
Great article! Lots of good book recommendations too 🙂
Babies can be affected by what you eat while breastfeeding. This is true for what you drink (alcohol is full of gluten) and what you eat. True celiacs can be effected my the very smallest trace amounts of gluten some even to the extent of food cooked in the same kitchen as gluten products from the small molecules of gluten on dishes or when flour gets into the air.
I couldn’t agree more!
Interesting thoughts. My son started showing signs of having issues at 9 months (he had only been eating solid foods for 2.5 months when the problems started). By 18 months we had a Celiac diagnosis. I have always struggled with what his trigger would have been. And his gut should have been perfectly healthy given that he had nothing but brrastmilk and fruits and vegetables at the time his problems started. I will be glad for more research so we can better understand how this came to be in his life.