
If you suffer from keratosis pilaris and wonder what’s behind those irritating and unsightly bumps on your skin, read this article. There may be a connection between keratosis pilaris and your diet. This post should not be construed as medical information. Please discuss any changes to your diet with your healthcare provider. Please see my disclosures and disclaimers.
If you’ve been navigating the ins and outs of a gluten-free diet due to celiac disease, non-celiac gluten sensitivity, or gluten intolerance, you’re likely highly attuned to how various foods make you feel, for better or worse.
However, you might not be aware of how this dietary shift can contribute to improving symptoms beyond the gut and may impact a skin condition, keratosis pilaris, that you once thought was unrelated.
This mostly harmless skin condition, sometimes called “chicken skin,” is characterized by tiny red and white bumps on the skin’s surface. These bumps typically affect areas where there are hair follicles, such as the top and back of arms, and almost look like goosebumps.
In this blog post, I’ll help you connect the likely link between keratosis pilaris and gluten. Please discuss any information with your doctor to ensure a proper diagnosis and treatment protocol. This article is for information purposes only and is not intended to be used as medical advice.

Keratosis Pilaris and Gluten
Research suggests that keratosis pilaris affects 50% to 80% of teenagers and 40% of adults at some point and is most common in adolescents.
This disorder manifests as small, non-inflamed bumps, giving the skin a goose-bump or chicken skin-like appearance. The bumps often occur on the upper arms, thighs, or buttocks.
There is no definitive research specifically connecting keratosis pilaris and celiac disease or other gluten disorders, making it challenging to ascertain direct causation. However, many people with celiac disease (including yours truly) have connected the dots in their own health, so anecdotal evidence exists. Why is this?

Some research says keratosis pilaris is associated with conditions such as atopic dermatitis, ichthyosis vulgaris, obesity, diabetes mellitus, and malnutrition. Malnutrition and nutrient deficiencies, like a Vitamin D deficiency, are strongly linked to unmanaged celiac disease as well.
Celiac disease is an autoimmune disorder triggered by the consumption of gluten, a protein found in wheat, barley, and rye. Every time someone with celiac disease eats gluten, their body’s immune response attacks the lining of the small intestine, impairing nutrient absorption and digestion.
While most people with celiac disease experience a slew of gastrointestinal symptoms, such as severe bloating, gas, diarrhea, and constipation, celiac can also come with a myriad of other symptoms, including nutrient deficiencies, that can lead to skin diseases (dermatitis herpetiformis, a skin manifestation of celiac disease), brain disorders, joint pain, and more. (Read: The 10 MOST Common Signs and Symptoms of Celiac Disease.)
My Keratosis Pilaris Story
I experienced red and white unsightly bumps running up and down my outer arms for years. The bumps didn’t hurt me, but I was self-conscious about them. Was it strange acne or a skin rash? Did I suffer from some sort of chronic inflammation? I didn’t know.
It wasn’t until I was diagnosed with celiac disease in 2012 that I began to connect the dots. After a few months of eliminating gluten from my diet, the bumps eventually disappeared. I went from having red and white bumps on my arms every day to having smooth and beautiful skin, all because I eliminated gluten.
This also happened on my tongue. I have an “unexplained” disorder called geographic tongue, which manifests as small crop circles on the tongue’s surface. My doctors and dentists told me it was harmless and the cause unknown. However, after going gluten-free, my geographic tongue began to dissipate, and I rarely have it anymore.
Like keratosis pilaris, malnutrition is a potential cause of geographic tongue, and once I got my celiac disease under control, all of these unexplained skin conditions were resolved.
Managing Keratosis Pilaris via a Gluten-Free Diet
Keratosis pilaris is challenging to treat because most people don’t understand its cause. While rubbing lotion on the red bumps can soothe irritated skin, it will do little to nothing to eliminate the condition. Lotions with perfumes or acne treatments may even irritate the skin and bumps.
If you have keratosis pilaris, I recommend talking to your healthcare provider to make a plan. Here are some items for your agenda:
(1) Get Tested for Celiac Disease
I highly recommend getting tested for celiac disease if you suffer from keratosis pilaris. Make sure you test for celiac disease BEFORE implementing a gluten-free diet because you must be eating gluten for a celiac test to be accurate.
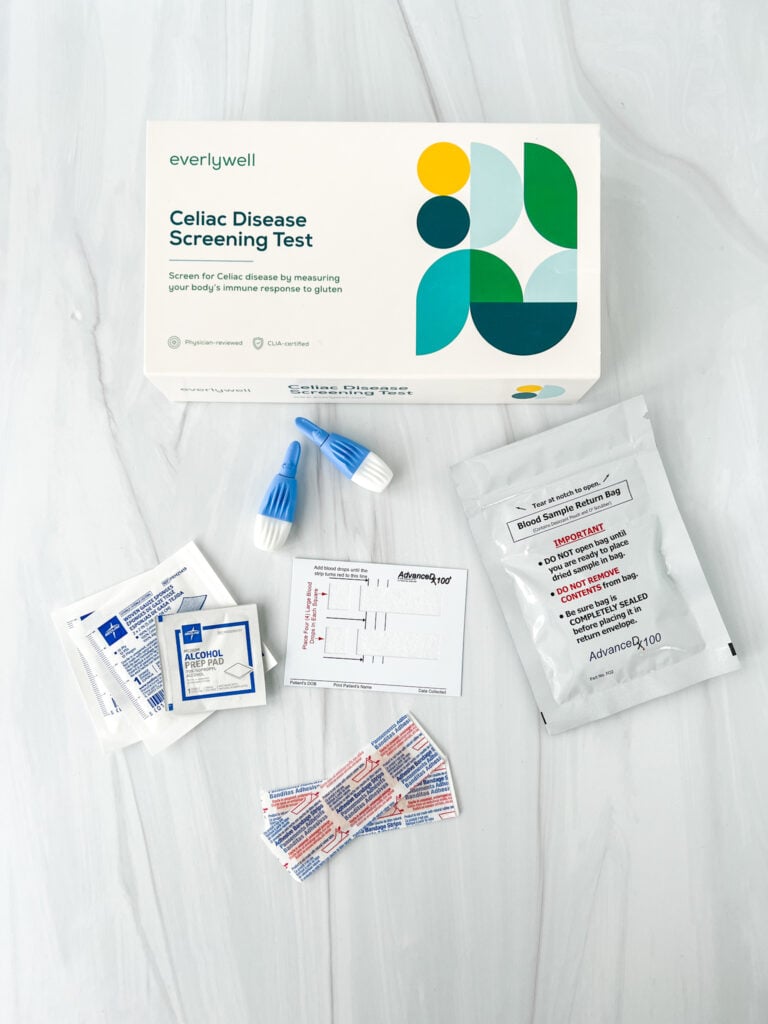
You can take this convenient at-home celiac test or talk to your doctor about getting screened for celiac disease. The at-home celiac screening test is the same blood test your doctor will give you, so if you take the test at home, be sure to share and discuss the results with your doctor.
If you test positive for celiac, your doctor will likely recommend an endoscopy procedure to examine the small intestine. If your small intestine is damaged in a way consistent with celiac disease, your doctor will diagnose you with the autoimmune disease.
At this time, you should eliminate gluten from your diet. As your gut heals and you absorb nutrients again, you will likely see your keratosis pilaris dissipate or clear.
If your celiac test is negative, it could be a sign of another disorder and could be related to poor diet, hormone imbalances, food sensitivities or food allergies. If you suspect it’s related to a food intolerance, I recommend reading this article, Do You Have Gluten Intolerance? How to Test for Non-Celiac Gluten Sensitivity, to give you a game plan for an elimination diet that will help you determine if you have gluten intolerance.
(2) Make Dietary Changes
The skin is the largest organ in your body and often mirrors what’s happening inside you. If your gut is in poor shape and you suffer from chronic digestive issues, your skin will likely show signs of trouble.
While eliminating gluten from your diet can potentially help manage keratosis pilaris, especially if you have celiac disease or gluten intolerance, your skin may still benefit from improving your diet.
Many experts recommend adopting a diet rich in fruits and dark leafy green vegetables, healthy fats (including omega-3 fatty acids), fiber-rich whole grains, and lean proteins, all of which can support digestion, gut health, and skin health.
Remember, the great Hippocrates, the father of modern medicine, once said, “All disease begins in the gut.” You will likely improve your whole-body health if you can improve your gut health.
(3) Take Probiotics
Along with improving your gut health, consider taking a high-quality daily probiotic. This will populate your gut with beneficial bacteria and help crowd out the bad bacteria that might be adversely impacting your health. Read more about probiotics in my article, The Benefits of Probiotics for Celiac Disease (and a list of gluten-free probiotic brands).
You could also eat probiotic-rich foods like lacto-fermented pickles, kimchi, and kombucha (fermented tea).
(4) Take Care of Your Skin
You can manage external symptoms by regularly and gently exfoliating the affected skin to remove dead skin cells, followed by gentle moisturizing. This will help keep the skin moisturized, reduce dry skin, and improve the appearance and texture of your skin.
Avoid using acne medications that dry out and irritate your skin. Remember, keratosis pilaris is not acne, even though it looks like it.
Whatever you do, don’t pick at your skin. Don’t try to pop the tiny bumps. They’re not pimples. And if you pick at the red and white bumps, you will likely cause more irritation and scarring.

Is Gluten the Missing Link?
No research conclusively suggests that keratosis pilaris and gluten are linked. However, there is evidence to suggest that keratosis pilaris can be linked to malnutrition, and nutritional deficiencies are a top symptom of unmanaged celiac disease.
For those with celiac disease or gluten intolerance, understanding these potential connections is vital. I recommend consulting with your healthcare provider, dermatologist, and/or gastroenterologist to provide you with clarity on the cause of your skin irritations and the potential role diet plays in it.
Remember, skin problems don’t happen on their own. If you want healthy skin, you must pay attention to your gut and whole-body health. As many say, skin is an inside job.
Related Articles
You might enjoy these related articles, too:
- STOP! Don’t Go Gluten-Free Until You Read This Article
- Can Gluten Cause Acne?
- Oral Manifestations of a Gluten Disorder: Mouth Sores, Tongue Spots, and Tooth Enamel Defects
- Can Celiac Disease Cause Hair Loss?
- 5 Connections Between Gluten and PCOS
- Candida and the Gluten Connection
- Leaky Gut and the Gluten Connection
- The Pros and Cons of a Gluten-Free Diet – Risks & Benefits
Leave a Comment